What Happens During the Second Stage Labor? A Guide to Baby’s Arrival
The second stage labor is the active pushing phase and begins when the cervix has reached full dilatation. It ends when the baby is removed from the vagina. The woman begins to push with each contraction to help the baby move down and out of the birth canal. It typically lasts anywhere from 30 minutes to two hours, depending on the individual mother’s experience and the position of the baby in relation to the pelvis. During this stage, hormones like oxytocin are released which stimulate uterine contractions. This can cause intense pressure, cramping, and pain, so many women find that it helps to focus on pushing with deep breaths as well as various birthing positions that open up the pelvis. Ultimately, this stage ends when the baby is delivered through vaginal birth or by cesarean section. Please keep reading for details on the following topics:
Characteristics of the second stage of labor
Delivery positions
The best positions to push
How a delivery vaginal delivery occurs
Advice on how to push during labor
Manual perineal protection at birth
Key Processes in the Second Stage of Labor
- Complete Cervical Dilation (10 cm):
- The first stage of labor ends when the cervix is fully dilated to 10 cm.
- The second stage begins, with the uterus pushing the baby downward toward the birth canal.
- Descent and Engagement of the Baby:
- The baby moves further into the birth canal, and the engagement occurs when the baby’s head reaches or passes the pelvic inlet.
- The baby rotates to an optimal position for delivery (usually head-down, with the face facing the mother’s back).
- Effacement and Crowning:
- The cervix may continue to thin out (efface) during this stage.
- The baby’s head gradually emerges from the birth canal, and the crown (top of the head) becomes visible at the opening of the vagina—this is called crowning.
- Pushing:
- The mother feels an intense urge to push as the baby’s head moves down the birth canal.
- The urge to push is triggered by the pressure of the baby’s head on the pelvic floor and rectum.
- Effective pushing helps to propel the baby downward with each contraction.
- The pushing process involves both involuntary (from contractions) and voluntary (from the mother’s effort) actions.
Stages of the Baby’s Delivery in the Second Stage
- Descent:
- The baby moves down through the birth canal, with each contraction.
- Flexion:
- The baby’s head typically flexes as it moves down, tucking the chin towards the chest to allow the smallest diameter of the head to pass through the birth canal.
- Internal Rotation:
- The baby rotates to a face-down position (if not already there) to fit through the pelvis.
- Extension:
- As the baby’s head emerges, the neck extends, and the face is delivered.
- Restitution:
- After the head is delivered, the baby’s shoulders rotate to align with the birth canal.
- External Rotation:
- The shoulders rotate externally after the head is delivered, allowing for the birth of the body.
- Birth of the Baby:
- The rest of the baby’s body (shoulders, arms, chest, legs) follows shortly after the head, often in one or two more pushes.
Types of Delivery in the Second Stage
- Vaginal Delivery:
- The most common and natural method where the mother pushes the baby out with the help of contractions.
- Assisted Delivery:
- In some cases, forceps or a vacuum extractor may be used to assist with the delivery of the baby, particularly if the baby is in distress or if the mother is too exhausted to push effectively.
- Cesarean Delivery:
- If complications arise, such as the baby not descending properly or fetal distress, a C-section may be necessary, though this is typically a decision made earlier in labor.
CHARACTERISTICS OF THE SECOND STAGE OF LABOR
The second stage of labor is characterized by several key aspects:
- Active Pushing: This stage begins when the cervix is fully dilated and ends with the birth of the baby. During this phase, the woman actively pushes with each contraction to assist the baby’s descent through the birth canal.
- Duration: The second stage can last anywhere from 20 minutes to several hours, depending on various factors such as the mother’s experience, the position of the baby, and the progress of labor.
- Intense Contractions: Contractions during the second stage are typically strong and frequent, aiding in pushing the baby downward. Contractions may become slower, shorter, or stop altogether to provide the mother with a rest period.
- Sensations: Women may experience sensations of pressure, cramping, and pain as the baby descends through the birth canal. This can vary in intensity from woman to woman. Nausea and vomiting may occur as the intensity of labor increases.
- Urge to Push: As the baby’s head enters the vagina, the woman may feel a strong urge to push, similar to the sensation of needing to have a bowel movement. Pressure is first felt on the rectum and then the perineum as the baby’s head presses down. With each pushing action, the baby progresses further down the birth canal.
- Physical Changes: As the baby’s head crowns, there may be an increase in the bloody show, and the vaginal tissues stretch to accommodate the baby’s passage. The woman may experience increased pain and burning sensation in the vagina as the baby’s head descends.
- Maternal Responses: Women may exhibit various responses during this stage, including feeling a surge of energy, becoming calmer and more focused, or feeling overwhelmed and requiring support from caregivers.
-
Delivery Positions: Different positions, such as lying on the back, side-lying, squatting, or kneeling, may be used to aid in the pushing process.
- Positioning:
- The mother may be encouraged to try different positions to help the baby move down the birth canal, including squatting, kneeling, sitting, or lying on her side.
- Positioning may be adjusted based on the mother’s comfort and the baby’s progress.
- Pain Management:
- Pain relief options such as epidurals, local anesthesia, or narcotics may still be used during this stage, though the intensity of contractions and pushing may still cause discomfort.
- Breathing techniques and relaxation may be employed to help manage pain and reduce fatigue.
- Monitoring the baby:
- Continuous monitoring of fetal heart rate is done to ensure the baby is tolerating the second stage of labor.
- A decrease in heart rate or other signs of fetal distress may lead to interventions.
- Coaching the mother:
- Healthcare providers may coach the mother on how to push effectively, encouraging short, strong pushes with each contraction.
- Rest periods between contractions allow the mother to regain energy before the next push.
THE WOMAN MAY
-
Experience a spurt of energy or ‘second wind’ as she approaches the final stage of childbirth.
- Feel calmer and regain a sense of purpose that she may have felt earlier in labor.
- Feel overwhelmed and require support from her birth companion and the midwife.
- Make grunting noises as she actively pushes with each contraction.
- Experience rupture of membranes if they are still intact, leading to the release of amniotic fluid.
- Feel panicked about needing to open her bowels at this stage and may require reassurance from her healthcare team.
- Become more energized and focused as she nears the end of labor and prepares to meet her baby.

DELIVERY POSITIONS
During the second stage of labor, various delivery positions may be utilized to aid in the birthing process. These positions include:
- On the Back: This position provides easier access to the vagina by healthcare providers and is commonly used in hospital settings.
- Side-Lying: The woman lies on her side, and her birthing companion can support her upper leg to widen the pelvis and assist with the baby’s descent.
- Hands and Knees: Being on hands and knees can help decrease back pain and may be beneficial for larger babies.
- Squatting: Squatting opens up the pelvis and is ideal for the pushing phase of birth.
- Upright/Sitting: Sitting on the bed, a birth ball, toilet, or rocking chair allows gravity to support the woman’s weight, helping the baby pass through the pelvis more quickly without putting excessive pressure on the perineum.
- Kneeling: Kneeling positions may also be used, allowing the woman to push effectively while maintaining balance and control.
- Standing: Some women may prefer to stand during the pushing phase, using their legs and gravity to aid in the baby’s descent.
- Using Props: Props such as birthing stools or balls may be used to support the woman in various positions and provide comfort during labor.
THE BEST POSITIONS TO PUSH
During the second stage of labor, various positions can optimize the pushing process. The best positions to push include:
- Kneeling: Kneeling on hands and knees can align the pelvis, allowing gravity to assist in the baby’s descent.
- Squatting: Squatting opens up the pelvis and utilizes gravity to aid in pushing. It can also provide leverage for the woman to push more effectively.
- Standing: Standing positions, such as leaning against a support or a partner, allow the woman to bear down with gravity’s assistance.
- Using a Birthing Stool: Sitting on a birthing stool can facilitate an open pelvic angle and provide support for effective pushing.
-
Leaning Over a Birthing Ball: Leaning forward over a birthing ball can relieve pressure on the perineum and encourage the baby’s descent.
HOW A DELIVERY VAGINAL DELIVERY OCCURS
During the second stage, the process typically unfolds as follows:
- Cervical Dilation: The cervix dilates to 10 centimeters to allow the baby’s head to pass through the birth canal.
- Pushing: The woman is encouraged to push during contractions while bearing down and relaxing between contractions to conserve energy.
- Baby’s Descent: As the woman pushes, the baby’s head begins to descend through the birth canal.
- Crowning: Once the baby’s head emerges at the vaginal opening, it is known as crowning. If needed, an episiotomy or a cut will be made to extend the opening of the vagina to facilitate the baby’s head out the vagina
- Delivery of the Head: The healthcare provider guides the baby’s head out gently, supporting it to prevent rapid expulsion, which can cause tearing.
- Delivery of the Shoulders and Body: Following the delivery of the head, the baby’s shoulders and body follow with gentle guidance from the healthcare provider.
- Cord Clamping and Cutting: Once the baby is fully delivered, the umbilical cord is clamped and cut.
- Initial Care: The baby is immediately dried and placed on the mother’s abdomen for skin-to-skin contact, which promotes bonding and helps regulate the baby’s temperature.
- Uterine Contractions: After the baby is delivered, the woman’s uterus continues to contract to expel the placenta and reduce bleeding. An injection will be administered to the woman’s thigh to provide medication (Pitocin) to keep the uterus firm and prevent bleeding.
- Placental Delivery: The placenta is delivered through the birth canal following the baby’s birth, typically within a few minutes to an hour after delivery.
- Perineal Care: The healthcare provider assesses the perineum for tears or lacerations and provides appropriate care, such as suturing if necessary.
-
Maternal Recovery: The woman is monitored closely for any signs of complications, and postpartum care is provided to support her recovery.
While pushing during the second stage, the woman should:
- Receive emotional support and encouragement to bear down when she feels the urge to do so.
- Be allowed to choose any position that enables her to push most effectively.
- Not push for longer than 2-3 hours to avoid excessive exhaustion.
- Relax the body and thighs to optimize pushing efforts.
- Concentrate and focus all energy on pushing with each contraction.
- Not worry about emptying the bowels or passing urine on the bed, as healthcare providers understand.
- Imagine the sensation of pushing out the largest stool possible to guide pushing efforts.
- Prop up the back and push the chin to the chest while taking deep breaths.
- Take deep breaths as contractions build and push throughout the contraction, exhaling slowly.
- Rest between contractions to conserve strength for the next round of pushing.
- Change positions if pushing isn’t progressing effectively.
- Avoid straining the upper body or face to prevent headaches or additional strain.
- The time it takes for baby to reach out of the vagina depends on the energy and effort placed on the pushing.
Manual Perineal Protection at Birth
Manual perineal protection at birth is an important practice that helps reduce the risk of perineal trauma and other childbirth-related injuries. Manual perineal protection at birth has been found to be an effective practice for reducing pain and injury for both mothers and infants. To prevent tears during childbirth, healthcare providers may employ several techniques:
-
Perineal Support: The midwife or doctor will use their hands to support both the woman’s perineum and the baby’s head as the baby is being birthed. This helps to ease the baby’s passage and reduce the risk of tearing.
- Controlled Breathing: The woman may be encouraged to slow down her breathing by panting during the pushing phase. This controlled breathing can help to manage the speed of the birth and reduce the likelihood of tearing.
- Episiotomy: In some cases, an episiotomy may be performed to create more space for the baby to be delivered. However, episiotomies are typically used judiciously and only when medically necessary.
- Perineal Massage: Massaging the perineum during labor can help to increase its flexibility and elasticity, reducing the risk of tearing. This massage can be performed by the midwife or doctor using lubrication.
Complications in the Second Stage
- Prolonged Second Stage:
- This is when the second stage lasts longer than expected (usually over 2 hours for first-time mothers or 1 hour for those who have delivered before). It can be caused by factors such as ineffective pushing, large baby size, or an unfavorable birth position.
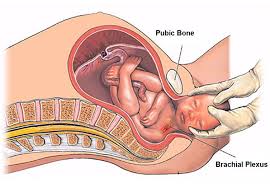
- Shoulder Dystocia:
- This is a rare but serious condition where the baby’s shoulder becomes stuck behind the mother’s pelvic bone after the head is delivered. Immediate intervention, such as specific maneuvers, is required.
- Fetal Distress:
- If the baby shows signs of distress (e.g., abnormal heart rate), interventions such as a cesarean delivery or forceps/vacuum assistance may be needed.
- Perineal Tears:
- The perineum (area between the vagina and anus) can tear during delivery, especially if the baby is large or if the mother is pushing too forcefully.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions. second stage second stage second stage second stage second stage second stage second stage


