Protecting Your Baby: How to Manage Rh Sensitization in Pregnancy
RH Sensitization is a growing problem in areas where humidity can be high and exposure to allergens can be frequent. It occurs when an individual develops an allergic reaction to their environment, typically due to exposure to environmental allergens or other triggers. Common symptoms of RH sensitization include skin irritation, sneezing, coughing, difficulty breathing, rhinitis and asthma-like symptoms. As RH sensitization can lead to serious long-term health problems, it is important for individuals living in these conditions to take preventive measures and get appropriate treatment if necessary. These may include changing the environment by controlling humidity levels and reducing mold growth as well as avoiding contact with known allergy triggers such as animal dander and pollen. In addition, medications or immunotherapy may be prescribed to help reduce the sensitivity of an individual’s immune system to these triggers. It is also important for individuals with RH sensitization to immediately seek medical help when they experience any of the ABOVE-MENTIONED symptoms as early diagnosis and treatment are key in managing this condition. Please keep reading for details on the following topics:
Consequences of rh sensitization
Diagnosing rh sensitization
Prevention of rh sensitization
Events contributing to the risk of blood mixing and sensitization during pregnancy
When to seek urgent medical care
Treatment of rh sensitization
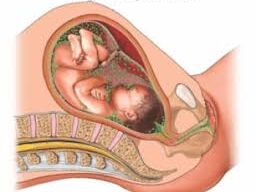
When an Rh negative mother delivers an Rh positive baby
As the two blood types mix, the mother’s immune system will create antibodies to attack the Rh positive blood type creating an Rh sensitization
CONSEQUENCES OF RH SENSITIZATION
Miscarriage/ still birth in subsequent pregnancies
Rh negative mother + Rh positive father = Rh positive child (Rh sensitization)
Rh negative mother + Rh negative father = Rh negative child (no Rh sensitization)
DIAGNOSING RH SENSITIZATION
Blood test at:
-24 to 28 weeks for the mother (indirect Coombs test)
-birth for the child (direct Coombs test)
PREVENTION OF RH SENSITIZATION
Rh immune globulin (such as RhoGAM) will be given:
Around week 28 of pregnancy
Within 72 hours of delivery of a Rh-positive baby
For every pregnancy
Events contributing to the risk of blood mixing and sensitization during pregnancy:
Trauma to the abdomen
Surgery in the abdomen
Placental problems
Miscarriage
Transfusion of Rh-positive blood in a Rh-negative person
TREATMENT OF RH SENSITIZATION
WHEN TO SEEK URGENT MEDICAL CARE
It is important to know when to seek urgent medical care, as delaying appropriate treatment can lead to further health complications. If you experience any of the following symptoms, you should seek medical help immediately. If you have any doubts about whether you should seek medical care, it is always better to err on the side of caution and consult with your doctor.
Unusual movement of the fetus
Suspected pregnancy or miscarriage
Incurred an accidental trauma to the abdomen
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

