Managing Postpartum Discomforts: Effective Strategies for Relief
Navigating the postpartum period can bring about various postpartum discomforts, but with the right knowledge and strategies, relief is within reach. From managing vaginal pain and perineal soreness to addressing pelvic bone pain and constipation, understanding how to alleviate these challenges is essential for new mothers. We’ll explore effective ways to tackle postpartum discomforts, ensuring a smoother transition into motherhood. Please keep reading for details on the following topics:
Managing postpartum discomforts
Vaginal pain and swelling
Perineal soreness
Pelvic bone pain
Constipation
Breast engorgement
Hemorrhoids
Reducing postpartum complications
When to seek urgent medical care
VAGINAL PAIN AND SWELLING

Vaginal pain and swelling postpartum is a very common postpartum discomforts for many women after childbirth. It can range from mild discomfort to intense pain and swelling. The most common causes are physical trauma during delivery, infection, or inflammation. Thankfully, there are many treatments available to help alleviate the symptoms of postpartum vaginal pain and swelling. These include rest, the application of warm compresses, sitz baths, and medications such as anti-inflammatories and antibiotics. In severe cases, surgery may be necessary. It is important to speak with a healthcare professional to determine the best course of action for your individual needs.
-
Vaginal pain and swelling occur as a result of trauma due to the vaginal delivery: During childbirth, the vaginal tissues undergo stretching and tearing, leading to pain and swelling. This trauma is a natural part of the birthing process but can cause discomfort postpartum.
- Tears will take a few weeks to heal: Tears or lacerations in the vaginal or perineal area may occur during delivery. These tears typically require time to heal, with the recovery period ranging from a few days to a few weeks, depending on the severity of the tear.
- Use over-the-counter Ibuprofen or Paracetamol: Ibuprofen and Paracetamol are common over-the-counter pain relievers. They can help alleviate the discomfort associated with vaginal pain and swelling. However, it’s essential to follow recommended dosage instructions and consult a healthcare professional if there are any concerns.
- Sit on a padded ring: Sitting on a padded ring, also known as a donut cushion, can help reduce pressure on the perineal area and provide relief from discomfort while sitting. This cushion distributes weight more evenly and can be especially helpful for individuals experiencing pain or swelling postpartum.
- Be sure to inform the doctor or midwife about any sign of infection: It’s crucial to monitor for signs of infection in the vaginal or perineal area, such as increased pain, swelling, redness, or abnormal discharge. Informing a healthcare provider promptly allows for timely evaluation and treatment if an infection is suspected.
- Apply ice pack to the area for 10 to 20 minutes at least 4 times daily can help reduce pain and swelling. Ice constricts blood vessels, which can decrease inflammation and numb the area, providing temporary relief. It’s typically recommended to apply ice for short intervals, several times a day, to avoid skin damage.
- Perform sitz bath for 4 to 6 times daily: A sitz bath involves sitting in warm water that covers the hips and buttocks. This can help soothe the perineal area, promote healing, and reduce discomfort. Sitz baths are often recommended multiple times a day to aid in recovery and provide relief from vaginal pain and swelling.
- Drink plenty fluids and eat fiber-rich foods to reduce the risk of constipation: Constipation can exacerbate discomfort in the perineal area. Staying hydrated and consuming foods high in fiber can help promote regular bowel movements, reducing the strain during bowel movements and minimizing discomfort.
- Avoid sexual intercourse before the vagina is adequately healed – Wait at least 4 to 6 weeks: Engaging in sexual intercourse too soon after childbirth can increase the risk of further trauma to the healing vaginal tissues and increase the likelihood of infection. It’s generally recommended to wait for 4 to 6 weeks, or until cleared by a healthcare provider, before resuming sexual activity.
-
Avoid douching (rinsing inside the vagina with hygienic products): Douching disrupts the natural balance of bacteria in the vagina and can increase the risk of infection. It’s unnecessary for vaginal hygiene and can lead to various complications, including irritation, inflammation, and an increased susceptibility to infections.

Perineal soreness, common postpartum discomforts that affects many people. It involves soreness in the area between the anus and genitals and can be caused by a variety of factors including childbirth, trauma, and certain medical conditions. Symptoms of perineal soreness can range from mild discomfort to severe pain and can have a significant impact on a person’s quality of life. Fortunately, there are a number of treatments available that can help relieve the symptoms and improve quality of life.
-
Apply ice pack for 10 to 20 minutes when necessary: It helps reduce swelling and discomfort in the perineal area following childbirth. Applying ice for short periods can numb the area and alleviate pain.
- Use warm water to clean the vagina without causing irritation. It’s important to maintain good hygiene to prevent infection, especially during the postpartum period when the body is healing.
- Use soft tissue when wiping: Soft tissue is gentle on the delicate skin of the perineum and reduces the risk of further irritation or injury. Avoid using rough or abrasive materials that could exacerbate discomfort.
- Wipe the vagina from the vagina towards the anus: This technique helps prevent the spread of bacteria from the anus to the vagina, reducing the risk of infection. It’s an important aspect of postpartum hygiene to maintain vaginal health.
- Perform sitz bath at least 4 times daily and after passing stool: Sitz baths involve sitting in warm water to soothe the perineal area and promote healing. They can help reduce pain, inflammation, and discomfort associated with childbirth-related trauma.
-
Be mindful that a tear to the perineum or an episiotomy takes many weeks to heal completely: Tears or episiotomies require time to heal properly. It’s essential to be patient and follow recommended postpartum care practices to support the healing process and avoid complications.
PELVIC BONE PAIN
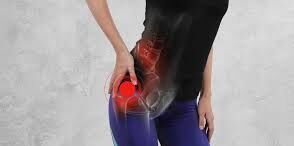
Pelvic bone pain is a common yet often misunderstood postpartum discomforts that can cause considerable discomfort and distress. It can be caused by a wide range of factors, including trauma, infection, discomfort of pregnancy, inflammation, delivery position adopted whilst in the delivery room and degenerative diseases. Symptoms can range from mild discomfort to severe pain and can be localized or widespread. Treatment options vary and may include physical therapy, medications, and lifestyle modifications. It is important to seek medical help if you are experiencing pelvic bone pain, as early diagnosis and treatment can lead to improved symptom relief and outcome.
-
Take pain medication as prescribed: Following the healthcare provider’s instructions regarding pain medication helps manage postpartum discomfort effectively. It’s essential to adhere to the prescribed dosage and frequency to alleviate pain without risking side effects.
- Apply ice packs to the area when necessary: Ice packs can provide relief from postpartum pain and swelling, particularly in areas like the perineum or abdomen. Applying ice packs for short durations as needed can help reduce inflammation and discomfort.
-
Have physical therapy: Physical therapy can play a crucial role in postpartum recovery, especially if there were complications during childbirth or if the individual experiences issues like pelvic floor weakness or abdominal separation (diastasis recti). Physical therapy sessions may include exercises to strengthen muscles, improve mobility, and alleviate pain, tailored to the individual’s specific needs and recovery goals.

Breast engorgement is one of the most uncomfortable postpartum discomforts in which a mother’s breasts become swollen, tender, and firm due to an increase in milk production. This condition can be caused by hormonal changes associated with pregnancy, breastfeeding, or weaning. While it can be uncomfortable and even painful, there are treatments that can help to reduce symptoms. Understanding the causes and treatments of breast engorgement can help to make the process easier and more manageable. To relieve breast engorgement:
-
Apply warm or ice packs to the breast when necessary can help relieve discomfort and reduce swelling associated with engorged breasts.
- Taking warm showers can help soothe the breast tissue and promote milk flow, providing relief from engorgement.
- Breastfeed using both breasts: Ensuring both breasts are emptied during feeding sessions helps maintain milk production balance and prevents further engorgement.
- Applying a cold washcloth to the breast before feeding can temporarily reduce milk supply and make it easier for the baby to latch on without overwhelming flow.
- Use firm support bras: A well-fitted, supportive bra can help alleviate discomfort by providing proper support to the engorged breasts.
- Take analgesia as needed: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain associated with engorgement.
-
Manual expression of breast milk: Gentle hand expression or pumping can help relieve pressure and facilitate milk removal, especially if the baby is unable to latch properly.
After childbirth, constipation, common postpartum discomforts that can be an uncomfortable and unpleasant experience for many mothers. This can be caused by a variety of factors, including hormonal changes and dietary shifts. It’s important to take steps to prevent constipation and know when to seek medical attention if needed. In this section, we’ll discuss the causes, symptoms, and treatments of constipation in postpartum mothers.
-
Dietary Fiber: Including foods rich in fiber in the diet can help increase bowel movement and promote regularity. Fiber adds bulk to stool, making it easier to pass, and it also helps prevent constipation.
- Fluid Intake: Increasing fluid intake helps to soften stool and facilitates bowel movements. Adequate hydration is essential for maintaining healthy digestion and preventing constipation.
- Sitz Bath: Sitz bath, a warm water bath taken in a sitting position, can help ease painful defecation, especially secondary to conditions like hemorrhoids. The warm water relaxes the muscles and promotes healing.
- Kegel Exercises: Kegel exercises are designed to strengthen the muscles of the pelvic floor. Performing these exercises regularly can help prevent pelvic floor disorders, improve bowel and bladder control, and promote overall pelvic health.
- Abundant Fruits and Vegetables: Fruits and vegetables are natural sources of fiber and hydration, both of which are essential for healthy bowel function. Including plenty of fruits and vegetables in the diet can aid digestion and prevent constipation.
- Stool Softeners: Stool softeners are medications that help soften stool, making it easier to pass. They are often prescribed to alleviate constipation and promote regular bowel movements.
- Regular Exercise: Regular physical activity can stimulate bowel movements and promote overall digestive health. Exercise helps to maintain muscle tone in the abdomen and can alleviate constipation.
-
Avoid Straining: Straining during bowel movements can lead to complications such as hemorrhoids, anal fissures, and pelvic floor dysfunction. Avoiding straining and adopting proper toileting habits, such as using a squatting position, can help prevent these issues.
HEMORRHOIDS

Childbirth is an incredible and life-changing experience but can also bring along its share of unexpected physical changes. One such change is the development of hemorrhoids, which can occur both during and after the pregnancy. Hemorrhoids can be painful and uncomfortable postpartum discomforts and can range from mild to severe. Understanding what causes them and how to manage them is key in making the postpartum period as comfortable as possible.
-
Carefully wipe the anus after passing stool: Gentle cleaning is important to prevent irritation or further injury to the anal area.
- Using soft tissue or baby wipes when wiping: Soft materials are less likely to cause irritation or exacerbate existing discomfort.
- Perform sitz bath as necessary: Sitting in warm water can soothe the area, reduce inflammation, and promote healing.
- Applying cold packs to the area for 10-20 minutes when necessary: Cold packs can help reduce swelling and provide temporary pain relief.
- Avoid sitting on hard surfaces: Hard surfaces can aggravate existing discomfort and slow down the healing process.
- Avoid sitting for prolonged periods of time: Prolonged sitting can increase pressure on the anal area, exacerbating symptoms.
- Avoid straining when passing stool: Straining during bowel movements can worsen conditions like hemorrhoids or anal fissures.
- Use stool softeners as prescribed: Stool softeners help ease bowel movements, reducing the likelihood of straining and further irritation.
-
Drink plenty fluids: Staying hydrated helps maintain soft stools, making them easier to pass and reducing the risk of constipation-related issues.
HOW TO REDUCE THE RISK OF POSTPARTUM COMPLICATIONS
Inform doctor of all pertinent information regarding past health history so that risks factors can be identified and managed accordingly. This emphasizes the importance of providing comprehensive information about one’s medical history to healthcare providers. This includes disclosing any pre-existing conditions, previous surgeries, allergies, medications, and family medical history. By sharing relevant health information, doctors can better assess the individual’s risk factors and tailor their care plan accordingly, optimizing postpartum health outcomes.
Attending postpartum clinic visits as scheduled underscores the significance of regular postpartum check-ups with healthcare providers. These appointments allow for monitoring of physical and emotional recovery after childbirth, addressing any concerns or complications that may arise, and providing guidance on postpartum care, breastfeeding, contraception, and parenting. By attending scheduled clinic visits, individuals can receive timely support and interventions to promote their well-being during the postpartum period.
Seek medical advice as soon as unusual symptoms are detected emphasizes the importance of promptly consulting a healthcare professional if experiencing any unusual or concerning symptoms during the postpartum period. This includes symptoms such as severe pain, heavy bleeding, fever, chest pain, difficulty breathing, headaches, mood changes, or any other signs of complications. Seeking timely medical advice allows for early detection, diagnosis, and management of potential health issues, ensuring optimal recovery and well-being for both the individual and their baby.
WHEN TO SEEK URGENT MEDICAL CARE
It is important to know when to seek urgent medical care, as delaying appropriate treatment can lead to further health complications. If you experience any of the following symptoms, you should seek medical help immediately. If you have any doubts about whether you should seek medical care, it is always better to err on the side of caution and consult with your doctor.
If having negative thoughts about self and baby
The desire to harm self, baby or others
Fainting
Pain to the chest, calf, head and abdomen
Difficulty breathing
Seizure
Vomiting
Fever
Heavy bleeding (soaking an entire pad with bright red blood in less than one hour)
Passing clots larger than the size of an egg
Passing tissue from the vagina
Pain, swelling and tenderness to the breast
Pain, burning or discomfort on urination
Swelling to the body
Difficulty seeing
Strange discharge from the vagina
Feeling of sadness and despair
Feeling unwell
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions. postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts postpartum discomforts

