Pelvic Exam: What to Expect and Its Importance for Women’s Health
The pelvic exam is an important part of a woman’s overall health and wellbeing. It is a routine procedure that can help detect any potential problems or health issues in the lower abdomen and pelvic area. During the exam, a healthcare provider will assess the size and shape of the pelvic area, the reproductive organs, and the external genitalia. It is important to stay informed about the pelvic exam and any risks associated with it so that you can make the best decisions for your health. Please keep reading for details on the following topics:
Overview of the pelvis
Preparing for a pelvic exam
What happens during a pelvic exam
Vaginal examination
Rectal exam

THE PELVIS
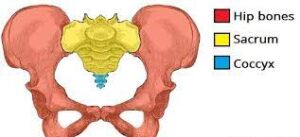
The pelvis is an important part of the human anatomy, located in the lower abdominal area. It provides support and stability for the entire body and is comprised of four bones: the sacrum, the ilium, the pubis, and the ischium. The pelvis also contains many ligaments and muscles that help to keep the body in balance, and its size and shape varies between men and women. Its intricate design allows us to move freely and comfortably, and it plays a vital role in childbirth, by providing a channel for the baby’s head to pass through.
HOW TO PREPARE FOR A PELVIC EXAM
A pelvic exam is an important part of a woman’s health and wellbeing. It’s important to be prepared for the experience and understand what to expect. This guide will provide an overview of the process, from gathering the necessary information to preparing for the exam and any follow-up care.
Best to have it done when the woman is not having a period
Do not douche or have intercourse 48 hours before the exam
Do not insert tampon or contraceptives into the vagina 48 hours before the exam
Avoid applying cream or other medication to the vagina 48 hours before the exam
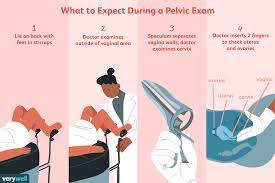
WHAT HAPPENS DURING A PELVIC EXAM

The woman will be asked to empty the bladder to avoid discomfort during the examination
A gown will be offered and bedsheet to provide privacy
The doctor will inquire about the woman’s health concerns
The doctor will listen to the heart and the lung sounds to determine any abnormalities
A breast exam will be conducted to detect the presence of lumps, secretions or any other abnormalities
The woman will be asked to lay on an examination table with the buttocks toward the end of the table and the legs opened with the knees bent
The abdomen will be palpated to feel the organs from the outside to determine the presence of abnormalities
The doctor will examine the exterior part of the vagina for abnormalities
The doctor will insert a metal instrument (called a speculum) inside the vagina to visualize inside
The woman will be encouraged to relax and breathe to ease discomfort
The doctor evaluates the structure reproductive organs for abnormalities
The doctor will pass a small brush and spatula inside and around the cervix to collect a sample of the cervical secretions to screen for cervical cancer and other infections
The secretions collected will be rubbed on a glass slide and labelled
The speculum will be removed after the test is complete
The doctor will insert two lubricated fingers into the vagina to examine the internal organs of the vagina such as the cervix
Gentle pressure will be applied to the lower abdomen with the other hand to examine the size and shape of uterus and ovaries for abnormalities
When the exam is complete the doctor will remove the fingers and offer a napkin to wipe the vulva
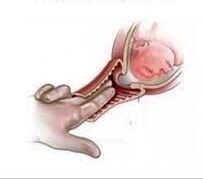
A lubricated finger will also be inserted into the rectum to assess for abnormalities
The finger will be removed and tissue will be offered to tidy self
The woman will be allowed to get dressed and results will be discussed afterwards
VAGINAL EXAMINATION (VE)
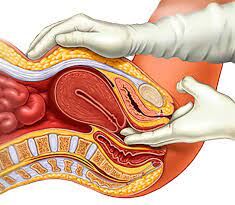
Vaginal exams are an important part of a woman’s health care. This procedure allows a doctor to evaluate the health of the reproductive system, including the vagina, cervix, and uterus. During a vaginal exam, the doctor will use a speculum to open the walls of the vagina in order to view the inside of the vagina and cervix. Next, two fingers will be inserted into the woman’s vagina, to examine the cervix. The doctor may also take a swab of the inside of the vagina to test for infection. Additionally, the doctor may take a Pap test to look for abnormal cells that can lead to cancer. It is important to discuss any concerns or questions you may have with your doctor before or during the vaginal exam.
REASONS WHY A VE IS PERFORMED
To examine the cervix
To determine how thin and how many centimeters dilated the cervix is
To confirm whether the membranes have ruptured
To determine the part of the baby which is presenting in the birth canal
To initiate labor by rupturing the membranes
To assess the woman’s progress in labor
Sweeping (or Stripping) the membranes
Making decisions about induction methods
To determine whether the pelvis is adequate to support a vaginal delivery
Vaginal exams during labor

Vaginal exams are a common part of the labor process for pregnant women. During a vaginal exam, a doctor or midwife will insert their fingers into the woman’s vagina to check the size and shape of the woman’s cervix. This helps them to determine if the woman is in active labor and if the baby is in the correct position for delivery. The doctor will also check to see how far the baby has descended into the birth canal. A vaginal exam can help the doctor or midwife to decide when it is time for the woman to push and when it is time to deliver the baby.
WHEN VE IS OFFERED
Here are the instances when a vaginal exam (VE) is offered to a pregnant woman:
-
On arrival to the hospital to determine the labor status (if a VE is not contraindicated): When a woman arrives at the hospital in labor, a vaginal exam may be performed to assess the status of her cervix and determine whether active labor has begun. This examination helps healthcare providers gauge the progress of labor, such as cervical dilation and effacement, and decide on appropriate management strategies.
- Every 4 hours during labor: During the active phase of labor, vaginal exams are often performed approximately every four hours to monitor cervical dilation, effacement, and fetal descent. These assessments provide valuable information about labor progress and help healthcare providers make decisions regarding pain management, interventions, and delivery timing.
- Before receiving pain medication during labor: Prior to administering pain medication or epidural anesthesia during labor, a vaginal exam may be conducted to evaluate cervical dilation and assess the woman’s eligibility for pain relief options. This examination helps healthcare providers determine the appropriate timing and dosage of pain medication and ensures safety during the administration process.
- If abnormal fetal heart readings are recorded during labor (this may be a sign that the baby is about to be born): In the presence of abnormal fetal heart rate patterns, which may indicate fetal distress or impending delivery, a vaginal exam may be performed to assess the progress of labor and determine if delivery is imminent. This examination helps healthcare providers evaluate the cervix, fetal position, and descent to prepare for potential interventions or assistance with childbirth.
- Before using a birth pool: Prior to utilizing a birth pool or water immersion for labor and delivery, a vaginal exam may be conducted to assess cervical dilation and ensure that labor has progressed to an appropriate stage for water birth. This examination helps healthcare providers determine the safety and feasibility of water immersion during labor and facilitates informed decision-making regarding birthing options.
- Before induction of labor: Before initiating labor induction, a vaginal exam may be performed to evaluate the cervix and assess its readiness for induction methods. This examination helps healthcare providers determine the appropriate timing and approach for labor induction, such as cervical ripening agents or oxytocin administration, based on cervical status and other clinical factors.
- If an abnormal NST is detected during labor (this may be a sign that the baby is about to be born): Nonstress tests (NSTs) are fetal monitoring tests commonly performed during labor to assess fetal well-being and response to uterine contractions. If an abnormal NST result suggests fetal compromise or distress, a vaginal exam may be conducted to evaluate labor progress, fetal position, and descent, and facilitate timely decision-making regarding delivery interventions or assistance.
-
To determine when to allow a woman to push in labor: During the second stage of labor, vaginal exams are often performed to assess cervical dilation, fetal station, and maternal pushing efforts. These examinations help healthcare providers determine the optimal timing for allowing the woman to begin pushing based on cervical readiness, fetal position, and maternal pushing effectiveness, thereby promoting efficient and safe childbirth.
RISKS OF A VE
Vaginal exams are an important part of many medical procedures, but they can also be associated with certain risks. While the risks associated with a vaginal exam are generally minimal, it is important for patients to understand the potential for complications and the steps their healthcare provider can take to minimize them. We’ll provide an overview of the risks associated with a vaginal exam and the steps your healthcare provider can take to reduce them.
-
Uncomfortable for the woman: Vaginal exams can be uncomfortable due to the pressure and manipulation of the sensitive tissues in the vaginal and rectal areas. This discomfort may cause anxiety or unease in some women during the exam.
- Painful: For many women, vaginal exams can be painful, especially if the cervix is not fully dilated or if there is significant pressure exerted during the exam. Pain levels can vary from woman to woman and depend on factors such as individual pain thresholds and the skill of the healthcare provider performing the exam.
- Distressing for primigravids and women who had previously experienced sexual abuse: Primigravid refers to women who are pregnant for the first time. For these women, the experience of a vaginal exam may be distressing due to the unfamiliarity of the procedure and the fear of the unknown. Similarly, women who have previously experienced sexual abuse may find the invasive nature of the exam triggering or traumatic.
- Embarrassing: Vaginal exams can be embarrassing for some women due to the intimate nature of the procedure and the exposure of their genitalia to healthcare providers. This embarrassment may stem from cultural or personal beliefs about modesty and privacy.
- Risk of infection to the mother and baby: Although rare, there is a small risk of introducing infection into the vaginal or rectal areas during a vaginal exam. This risk increases if proper hygiene practices are not followed or if the healthcare provider’s hands or equipment are contaminated.
- Errors: Vaginal exams require skill and precision on the part of the healthcare provider to accurately assess cervical dilation, fetal position, and other important indicators of labor progress. Errors in conducting the exam, such as incorrect measurement of cervical dilation or misinterpretation of findings, can lead to inaccurate assessments and potentially unnecessary interventions.
- Accidental rupture of membranes: During a vaginal exam, there is a risk of accidentally rupturing the amniotic sac (membranes) surrounding the baby, especially if the cervix is already dilated. This unintended rupture of membranes can lead to premature labor or complications such as infection.
-
Traumatic for past victims of sexual abuse or assault: Women who have experienced sexual abuse or assault in the past may find vaginal exams particularly traumatic due to the invasive nature of the procedure and the association with past trauma. The exam may trigger feelings of fear, vulnerability, or helplessness in these women, requiring sensitivity and support from healthcare providers.
ALTERNATIVES TO A VE
When a woman goes into labor, there are a variety of options to consider when it comes to her care. One of the most important decisions to make is whether or not to have a traditional vaginal exam. For some women, this option may not be suitable or desired. Luckily, there are alternative options available to ensure that the pregnant woman gets the care she needs. Here are some of the alternative options to a traditional vaginal exam during labor.
-
Watching and listening to the woman: This refers to the healthcare provider observing and paying close attention to the woman’s behavior, verbal cues, and vital signs during labor. By carefully observing the woman’s facial expressions, body language, and vocalizations, healthcare providers can gain valuable insights into her physical and emotional state. Additionally, listening to the woman’s verbal communication allows healthcare providers to understand her concerns, preferences, and needs during labor. This attentive approach enables healthcare providers to provide personalized care, offer reassurance, and respond promptly to any changes or complications that may arise.
- The presence of a purple color around the anus: This observation may indicate a condition known as purpura, which is characterized by the appearance of purple-colored spots or patches on the skin. In the context of labor and childbirth, the presence of a purple color around the anus may suggest increased pressure on the pelvic floor muscles and blood vessels during contractions. This pressure can restrict blood flow to the area, causing blood vessels to dilate and resulting in the characteristic purple discoloration. Healthcare providers may monitor this sign as an indication of progress during labor and assess its significance in relation to the woman’s overall well-being and the progression of labor.
-
Hotness or coldness to the legs: Sensations of hotness or coldness in the legs may occur during labor and childbirth as a result of changes in blood flow and circulation. During contractions, blood flow to the legs may decrease temporarily as blood is redirected to the uterus and other vital organs involved in labor. This can cause the legs to feel cooler than usual. Conversely, after contractions subside or during periods of increased blood flow, the legs may feel warmer or experience sensations of heat. Healthcare providers may observe and assess these sensations as part of their evaluation of the woman’s circulation, comfort, and overall well-being during labor. Any significant changes in temperature or sensation may prompt further assessment and intervention to ensure the woman’s safety and comfort throughout the labor process.
RECTAL EXAM
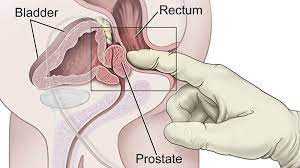
Rectal exam is a medical procedure used to examine the lower digestive tract. It involves the insertion of a lubricated, gloved finger into the rectum in order to feel for any abnormalities. The exam is typically performed by a doctor or a nurse practitioner, and it is an important part of the diagnostic process for many conditions, including cancer and infections. In addition, the exam can be used to assess the overall health of the lower digestive tract. Rectal exam is a relatively quick and painless procedure that can provide valuable information to your healthcare provider.
WHEN A RECTAL EXAM IS INDICATED
-
To identify abnormal mass in the anus, rectum, or ovaries: A rectal exam involves the insertion of a lubricated, gloved finger into the rectum to feel for any abnormal masses or growths in the anal canal, rectum, or nearby organs such as the ovaries. This examination helps in detecting conditions such as hemorrhoids, anal or rectal polyps, rectal tumors, or ovarian cysts or tumors. Identifying these abnormalities early is crucial for timely diagnosis and appropriate management.
- To collect stool specimen: During a rectal exam, healthcare providers may obtain a small sample of stool from the rectum for laboratory analysis. This stool specimen can be examined for various purposes, including detecting the presence of blood, mucus, parasites, bacteria, or other abnormal substances. Stool testing aids in diagnosing gastrointestinal conditions such as infections, inflammatory bowel disease, colorectal cancer, or malabsorption disorders.
- To identify the source of rectal bleeding: Rectal exams are often performed in individuals who present with symptoms of rectal bleeding or blood in the stool. By visually inspecting the anal canal and rectal mucosa and palpating the area for abnormalities, healthcare providers can determine the source and severity of rectal bleeding. Potential causes of rectal bleeding include hemorrhoids, anal fissures, rectal ulcers, colorectal polyps, inflammatory bowel disease, or colorectal cancer. Identifying the underlying cause of rectal bleeding is crucial for guiding further diagnostic evaluation and treatment.
- To determine the extent of a 3rd or 4th degree vaginal tear: Following childbirth, some women may experience perineal tears that extend into the vaginal wall and surrounding tissues. In cases where a severe tear involving the anal sphincter muscles (3rd or 4th degree tear) is suspected, a rectal exam may be performed to assess the extent of the tear and its potential impact on bowel function and pelvic floor integrity. This examination helps healthcare providers determine the appropriate management approach, which may include surgical repair or referral to a specialist for further evaluation and management.
- For persons who have a change in bowel habits: Individuals who experience changes in their bowel habits, such as increased frequency, urgency, constipation, diarrhea, or unexplained rectal discomfort, may undergo a rectal exam to evaluate rectal tone, presence of fecal impaction, rectal masses, or other abnormalities contributing to altered bowel function. This assessment guides diagnostic evaluation and treatment planning for gastrointestinal symptoms or concerns.
-
For persons who are constipated: Rectal exams may be indicated for individuals experiencing constipation, as this examination allows healthcare providers to assess rectal tone, presence of fecal impaction, rectal masses, or other abnormalities that may contribute to difficulty with bowel movements. By identifying the underlying cause of constipation, such as rectal obstruction, pelvic floor dysfunction, or neurological issues, healthcare providers can tailor treatment strategies to alleviate symptoms and improve bowel function.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

