Managing Kidney Failure: Treatment Options and Lifestyle Changes
Kidney failure, also known as renal failure or End-stage kidney disease, is a medical condition in which the kidneys no longer function optimally to perform their essential functions, leading to a build-up of waste and fluid in the body. Consequently, the kidneys are unable to remove waste substances from the blood. The kidneys are two bean-shaped organs located at either side of the back, below the rib cage. Their primary role is to filter excess fluid, electrolytes and waste from our blood and excrete them through urine. In addition, they help to regulate our body’s hormones and control blood pressure. When kidney failure occurs, these vital functions are reduced or completely stopped, leading to serious health complications. Please keep reading for details on the following topics:
Classification of kidney failure
Symptoms of renal disease
Causes of renal disease
Complications of renal disease
Diagnosis of renal disease
Treatment of renal disease
Prevention of renal disease
Classification of Kidney Failure
There are two main types:
-
Acute Kidney Injury: This is a sudden loss of kidney function that occurs over a short period of hours to days, often due to factors such as decreased blood flow to the kidneys, urinary tract blockage, or certain medications. Acute kidney injury is reversible and can be resolved with prompt treatment. Symptoms may include nausea, vomiting, fatigue, weakness, confusion and decreased urine output.
-
Chronic Kidney Disease: This is a gradual and irreversible decline in kidney function over months or years, usually resulting from underlying health conditions such as diabetes, high blood pressure, or chronic kidney diseases. Chronic kidney failure may eventually progress to end-stage kidney disease, where kidney function is severely impaired causing a build-up of toxins in the body which can cause further health complications such as uremia (build up of toxic waste products) and hypertension (high blood pressure) and requires ongoing medical intervention, such as dialysis or kidney transplantation. Common symptoms include swelling in the lower limbs and face due to water retention caused by impaired kidney function, fatigue, anemia (low red blood cell count), increased urination at night and poor appetite.
Causes of renal disease
Renal disease can result from various underlying conditions and factors that impair the normal function of the kidneys. Here are some common causes:
- Diabetes is one of the leading causes of kidney failure. Over time, high blood sugar levels associated with diabetes can damage the small blood vessels and structures in the kidneys, leading to diabetic nephropathy, a type of chronic kidney disease (CKD) that can progress to kidney failure.
- High Blood Pressure (Hypertension): Chronic uncontrolled high blood pressure can damage the blood vessels in the kidneys, impairing their ability to filter waste and regulate fluid and electrolyte balance.
- Glomerulonephritis refers to inflammation of the glomeruli, the tiny filtering units in the kidneys. Chronic glomerulonephritis can lead to progressive kidney damage and eventual kidney failure. It may result from autoimmune disorders, infections, or other immune-mediated conditions.
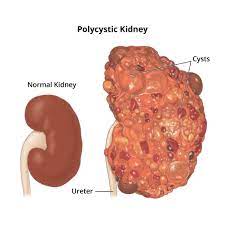
- Polycystic Kidney Disease (PKD) is a genetic disorder characterized by the growth of numerous fluid-filled cysts in the kidneys. These cysts can gradually replace healthy kidney tissue, impairing kidney function and leading to kidney failure over time.
- Chronic or recurrent kidney stones can obstruct the urinary tract, leading to complications such as kidney damage, infection, and inflammation. In some cases, severe or untreated kidney stone disease can contribute to kidney failure.
- Blockages or obstructions in the urinary tract, such as from enlarged prostate, kidney stones, tumors, or congenital abnormalities, can prevent urine from draining properly from the kidneys. Prolonged obstruction can lead to kidney damage and eventual kidney failure.
- Autoimmune Disorders: Certain autoimmune diseases, such as lupus nephritis, IgA nephropathy, and vasculitis, can cause inflammation and damage to the kidneys, leading to chronic kidney disease and eventual kidney failure.
- Severe or recurrent infections, such as kidney infections (pyelonephritis) or certain viral infections, can cause inflammation and damage to kidney tissue, contributing to kidney failure.
- Medications and Toxins: Certain medications, toxins, and environmental exposures can damage the kidneys and impair their function. Examples include long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), certain antibiotics, chemotherapy drugs, heavy metals, and environmental pollutants.
-
Acute Kidney Injury (AKI) can result from sudden and severe damage to the kidneys, often due to factors such as decreased blood flow (hypoperfusion), dehydration, severe infections, or drug toxicity.
Symptoms of renal disease
Symptoms can vary depending on the type and severity of the condition. Here are some common symptoms associated with both acute and chronic kidney disease:
- Swelling: Also known as edema, swelling can occur in the legs, ankles, feet, face, or other parts of the body due to fluid retention caused by impaired kidney function.
- Fatigue: Feeling unusually tired or weak, even with adequate rest, is a common symptom of kidney failure.
- Decreased Urine Output: Oliguria, or decreased production of urine, can occur. In some cases, urine output may stop altogether.
- Nausea and Vomiting: Persistent nausea and vomiting can be accompanied by loss of appetite.
- Confusion: Changes in mental alertness or confusion may occur, particularly in cases of severe kidney failure where waste products build up in the bloodstream.
- Itching: Pruritus, or persistent itching of the skin, can occur in kidney failure due to the build-up of toxins in the bloodstream.
- High Blood Pressure: Hypertension, or high blood pressure, is a common complication and may contribute to further kidney damage.
- Weight Loss: Unintended weight loss may occur in individuals with kidney failure due to loss of appetite, nausea, and changes in metabolism.
- Changes in Urination: Kidney failure can lead to alterations in urination patterns. This may include more frequent urination, often with greater amounts of pale urine, or less frequent urination with smaller amounts of dark-colored urine. Hematuria, or blood in the urine, may also occur.
- Bone Damage: Chronic kidney failure can lead to weakened bones and increased risk of fractures due to imbalances in calcium and phosphorus levels, as well as decreased production of vitamin D.
- Shortness of Breath or Difficulty breathing may occur due to fluid accumulation in the lungs, known as pulmonary edema, which can develop as a complication of the disease.
- Darkening of the Skin: Changes in skin color or darkening of the skin, particularly around the eyes or on the legs, may occur due to build-up of waste products in the bloodstream.
It’s important to note that individuals with kidney failure may not experience all of these symptoms, and some symptoms may be more prominent than others. Additionally, symptoms can vary depending on individual factors such as underlying health conditions and the stage of kidney failure. If you experience any of these symptoms, it’s essential to seek medical attention for proper evaluation and management.
Complications of renal disease can significantly impact an individual’s health and quality of life. Here are some common complications:
- Elevated Levels of Urea in the Blood (Azotemia): Kidneys normally filter waste products, including urea, from the blood. In kidney failure, urea and other waste products can build up in the bloodstream, leading to a condition known as azotemia.
- Elevated Levels of Potassium in the Blood (Hyperkalemia): Healthy kidneys regulate potassium levels in the body. In kidney failure, potassium may accumulate in the blood, leading to hyperkalemia. This can cause abnormal heart rhythms and other cardiovascular complications.
- Fluid Overload (Edema): Kidneys play a vital role in regulating fluid balance in the body. In kidney failure, the kidneys may not effectively remove excess fluid, leading to fluid retention and swelling (edema) in the legs, arms, face, or other parts of the body.
- Cardiovascular Disease: Kidney failure is associated with an increased risk of cardiovascular complications, including coronary artery disease, heart failure, high blood pressure (hypertension), and abnormal heart rhythms. These cardiovascular complications can significantly impact morbidity and mortality in individuals with kidney failure.
- Anemia: Healthy kidneys produce erythropoietin, a hormone that stimulates the production of red blood cells in the bone marrow. In kidney failure, erythropoietin production may be decreased, leading to anemia (low red blood cell count). Anemia can cause fatigue, weakness, shortness of breath, and other symptoms.
- Bone Disease: Kidney failure can lead to disturbances in mineral and bone metabolism, resulting in bone disease. These disturbances may include abnormalities in calcium, phosphorus, and vitamin D metabolism, leading to conditions such as renal osteodystrophy, osteoporosis, and bone fractures.
- Electrolyte Imbalances: Healthy kidneys help regulate electrolyte levels in the body, including sodium, potassium, calcium, and phosphorus. In kidney failure, electrolyte imbalances may occur, leading to complications such as muscle weakness, cramps, cardiac arrhythmias, and seizures.
- Metabolic Acidosis: Kidney failure can impair the excretion of acids from the body, leading to metabolic acidosis. This condition occurs when there is an excess of acid in the body, resulting in symptoms such as fatigue, weakness, confusion, and abnormal breathing patterns.
- Fluid in the Lungs (Pulmonary Edema): In severe cases of fluid overload, excess fluid may accumulate in the lungs, causing pulmonary edema. This can lead to symptoms such as shortness of breath, difficulty breathing, and coughing.
-
Impaired Immune Function: Kidney failure can impair the function of the immune system, leading to an increased risk of infections. Individuals with kidney failure may be more susceptible to bacterial, viral, and fungal infections, which can further complicate their health status.
How renal disease is diagnosed
Diagnosis typically involves a combination of medical history, physical examination, laboratory tests, imaging studies, and sometimes kidney biopsy. Here’s an overview of the diagnostic process:
- Medical History and Physical Examination: The healthcare provider will take a detailed medical history, asking about symptoms, risk factors, and any underlying medical conditions that could contribute to kidney dysfunction. A physical examination may also be performed to assess for signs of kidney disease, such as swelling (edema), hypertension, and changes in urine output.
- Blood Tests: Blood tests are essential for assessing kidney function and detecting abnormalities in blood chemistry. Common blood tests used in the diagnosis of kidney failure include:
- Serum Creatinine: Creatinine is a waste product produced by muscle metabolism and excreted by the kidneys. Elevated levels of serum creatinine indicate impaired kidney function.
- Blood Urea Nitrogen (BUN): BUN is another waste product that accumulates in the blood when kidney function is impaired. Elevated BUN levels can indicate kidney dysfunction.
- Glomerular Filtration Rate (GFR): GFR is a measure of kidney function that estimates how well the kidneys are filtering waste from the blood. A decreased GFR indicates reduced kidney function.
- Urine Tests: Urinalysis and urine protein tests can provide valuable information about kidney function and detect abnormalities in urine composition. Urinalysis may reveal the presence of blood, protein, or abnormal levels of electrolytes and waste products.
- Imaging Studies: Imaging tests such as ultrasound, CT scan, or MRI may be performed to visualize the structure and size of the kidneys, as well as to detect any abnormalities such as kidney stones, tumors, or obstruction of the urinary tract.
- Kidney Biopsy: In some cases, a kidney biopsy may be performed to obtain a small sample of kidney tissue for microscopic examination. A kidney biopsy can help diagnose the underlying cause of kidney dysfunction, assess the severity of kidney damage, and guide treatment decisions.
-
Additional Tests: Depending on the suspected cause, additional tests may be ordered to evaluate specific aspects of kidney function or identify underlying conditions. These may include tests for autoimmune disorders, infections, electrolyte imbalances, or genetic abnormalities.
Treatment of renal disease

The treatment depends on the type of kidney failure (acute or chronic), the underlying cause, the severity of kidney dysfunction, and individual patient factors. Here’s an overview of the treatment options for kidney failure:
- Management of Underlying Conditions: If kidney failure is caused by an underlying medical condition such as diabetes, high blood pressure, autoimmune disorders, or urinary tract obstruction, managing these conditions is essential for preventing further kidney damage and preserving kidney function. This may involve lifestyle modifications, medications, and other targeted therapies.
- Dietary modifications may be recommended to help manage symptoms and complications of kidney failure, such as fluid retention, electrolyte imbalances, and proteinuria. This may include reducing sodium intake, limiting potassium and phosphorus-rich foods, and adjusting protein intake based on individual needs.
- Medications may be prescribed to manage symptoms, control underlying conditions, and prevent complications of kidney failure. Commonly prescribed medications may include:
- Blood Pressure Medications: Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are often used to control high blood pressure and reduce proteinuria, thereby slowing the progression of kidney disease.
- Diuretic medications may be prescribed to help remove excess fluid from the body and manage symptoms of fluid overload, such as edema and shortness of breath.
- Erythropoiesis-Stimulating Agents (ESAs) may be used to treat anemia associated with kidney failure by stimulating the production of red blood cells in the bone marrow.
- Phosphate Binders may be prescribed to help lower blood phosphate levels and prevent complications of hyperphosphatemia, such as bone disease.
- Calcium Supplements and Vitamin D Analogs: These may be prescribed to help manage disturbances in calcium and vitamin D metabolism associated with kidney failure.
- Dialysis is a medical procedure that helps remove waste products and excess fluid from the blood when the kidneys are no longer able to do so adequately. There are two main types of dialysis:
- Hemodialysis involves using a machine (dialyzer) to filter the blood outside the body. The blood is pumped through a dialyzer, where waste products and excess fluid are removed, and then returned to the body.
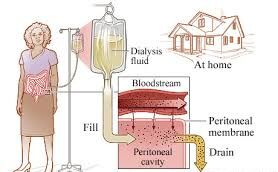
- Peritoneal dialysis involves using the lining of the abdomen (peritoneum) as a natural filter. A special solution (dialysate) is infused into the abdomen through a catheter, and waste products and excess fluid pass from the blood vessels into the dialysate, which is then drained out of the body.
- Kidney transplantation is considered the best long-term treatment option for many patients with end-stage kidney disease. During a kidney transplant, a healthy kidney from a donor (living or deceased) is surgically implanted into the recipient’s body to replace the failed kidneys. Kidney transplantation offers the potential for improved quality of life and survival compared to long-term dialysis.
-
Symptom Management and Supportive Care: In addition to medical and surgical interventions, symptom management and supportive care are important aspects of treating kidney disease. This may include addressing symptoms such as pain, fatigue, itching, and sleep disturbances, as well as providing emotional support and counseling to patients and their families.

Preventing renal disease involves adopting healthy lifestyle habits and managing underlying medical conditions that can contribute to kidney damage. Here are some strategies for preventing kidney failure:
- Control medical conditions such as diabetes, high blood pressure (hypertension), and autoimmune disorders that can increase the risk of kidney damage. Follow treatment plans prescribed by healthcare providers, including taking medications as prescribed, monitoring blood sugar and blood pressure levels regularly, and making necessary lifestyle changes.
- Follow a balanced diet that is low in sodium, saturated fats, and cholesterol, and rich in fruits, vegetables, whole grains, and lean proteins. Limit intake of processed foods, sugary beverages, and foods high in phosphorus and potassium, which can stress the kidneys and contribute to kidney damage.
- Drink plenty of water throughout the day to help maintain proper hydration and support kidney function. Adequate hydration helps flush toxins and waste products from the body and reduces the risk of kidney stones and urinary tract infections.
- Engage in regular physical activity to help maintain a healthy weight, lower blood pressure, improve cardiovascular health, and reduce the risk of chronic conditions such as diabetes and obesity that can contribute to kidney damage.
- Quit smoking and limit alcohol consumption, as smoking and excessive alcohol intake can damage blood vessels, impair kidney function, and increase the risk of kidney disease and other health problems.
- Use medications as directed by healthcare providers and avoid over-the-counter medications, herbal supplements, and illicit drugs that can be harmful to the kidneys. Be cautious with nonsteroidal anti-inflammatory drugs (NSAIDs) and other medications that can cause kidney damage with prolonged use or at high doses.
- Practice stress-reduction techniques such as mindfulness, meditation, yoga, deep breathing exercises, and relaxation techniques to help manage stress and promote overall health and well-being.
- Schedule regular check-ups with healthcare providers to monitor kidney function, blood pressure, blood sugar levels, and other markers of health. Early detection and treatment of kidney disease and underlying conditions can help prevent progression to kidney failure.
- Minimize exposure to environmental toxins, chemicals, heavy metals, and pollutants that can damage the kidneys and other organs. Follow safety guidelines and protective measures when working with hazardous substances.
-
Be aware of your family history of kidney disease and other medical conditions that can increase the risk of kidney failure. Discuss any concerns or risk factors with healthcare providers and take proactive steps to prevent kidney damage.
👉CLICK TO CHECK OUT A STORY ON KIDNEY FAILURE
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

