Preparing for Induction of Labor: What to Expect During the Process
Induction: The use of medications or other methods to bring on (induce) labor. Labor is the physiological process through which a fetus exits the uterus and vaginally out of the mother’s body during childbirth. It begins with contractions of the uterus and ends with cervical dilatation and delivery of the newborn. Labor consists of several stages; each one has distinct characteristics that allow medical personnel to recognize it accurately and intervene as needed. Please keep reading for details on the following topics related to induction of labor:
The difference between induction and augmentation of labor
Reasons for inducing labor
Risks or complications of inducing labor
Methods of inducing labor
Contraindications to inducing labor
The difference between induction and augmentation of labor
Induction of labor is the process by which a woman’s body is prepared for childbirth. With induction of labor, labor is initiated using non-natural efforts. During induction, a physician will use medications or other methods to cause the body to go into labor. The purpose of labor induction is to start labor before it would begin naturally. In some cases, such as when a mother’s health or that of her baby is at risk, inducing labor may be necessary.
Meanwhile, augmentation of labor uses efforts to increase contractions. Augmentation of labor occurs when there are difficulties with progress during natural labor or when conditions warrant that progression be sped up due to potential risk factors present in mother or baby. During augmentation, medical staff can provide drugs to stimulate uterine contractions, break an unripe cervix, or adjust the fetal position in order to help facilitate a successful vaginal birth. Augmentation of labor can significantly reduce complications for both mother and baby but must be carefully monitored throughout its duration in order to avoid overstimulation and ensure maximal safety for both parties involved in delivery.
REASONS FOR INDUCING LABOR
Reasons for inducing labor include various medical conditions and situations where it is deemed necessary to initiate labor artificially. Here are some common reasons:
- Post-term Pregnancy: When pregnancy extends beyond 4 days past the due date (typically 40+5 weeks), induction may be recommended to reduce the risk of complications associated with prolonged pregnancy.
- Post-mature Pregnancy: Similar to post-term pregnancy, post-mature pregnancy occurs when pregnancy lasts beyond 41 to 42 weeks. Induction may be considered to prevent potential risks to both the mother and the baby.
- Premature Rupture of Membranes: If the amniotic sac ruptures (water breaks) before the onset of labor, inducing labor may be necessary to reduce the risk of infection or other complications.
- Infection in the Uterus: In cases of intrauterine infection, such as chorioamnionitis, inducing labor may be recommended to prevent the spread of infection to the mother or the baby.
- Fetal Growth Restriction: When the fetus is not growing adequately in the womb (intrauterine growth restriction), inducing labor may be necessary to deliver the baby and ensure proper monitoring and care.
- Oligohydramnios: Low levels of amniotic fluid surrounding the baby (oligohydramnios) may indicate potential fetal distress. Inducing labor can help ensure the baby’s safety and well-being.
- Gestational Diabetes: If a woman develops gestational diabetes during pregnancy and her blood sugar levels cannot be adequately controlled, induction may be recommended to prevent complications for both the mother and the baby.
- High Blood Pressure Disorders: Conditions such as preeclampsia or gestational hypertension may require induction to prevent the progression of complications that could endanger the health of the mother or the baby.
- Placental Abruption: In cases where the placenta separates from the uterine wall prematurely (placental abruption), induction may be necessary to deliver the baby promptly and prevent further complications.
-
Fetal Demise: In the tragic event of fetal demise (stillbirth), induction of labor is necessary to deliver the baby and provide closure for the parents.
RISKS OR COMPLICATIONS OF INDUCING LABOR
Inducing labor carries certain risks and potential complications, which healthcare providers must consider before proceeding. Here are some of the risks associated with inducing labor:
- Prolapse of the Umbilical Cord: Inducing labor may increase the risk of umbilical cord prolapse, where the cord slips through the cervix ahead of the baby, potentially cutting off the baby’s oxygen supply.
- Severe Pain: Induced contractions can be more intense and painful than spontaneous labor contractions, leading to increased discomfort for the mother.
- Uterine Rupture: In some cases, inducing labor may increase the risk of uterine rupture, especially in women who have had previous uterine surgeries such as cesarean sections.
- Failure to Progress: Inducing labor may result in a failure to progress, where the cervix does not dilate sufficiently or labor stalls, necessitating a cesarean section delivery.
- Fetal Distress: Medications used to induce labor may cause excessive contractions, reducing blood flow to the placenta and compromising the baby’s oxygen supply, leading to fetal distress.
- Infection Risk: Some methods of labor induction, such as rupturing the membranes or using internal monitors, increase the risk of infection for both the mother and the baby.
- Heavy Bleeding: Inducing labor may increase the risk of postpartum hemorrhage (excessive bleeding after delivery), particularly if labor progresses rapidly or if there are complications during childbirth.
- Maternal Exhaustion: Prolonged or intense labor induced artificially may lead to maternal exhaustion, which can affect the mother’s ability to cope with labor and increase the likelihood of interventions such as assisted delivery.
- Hyperstimulation: Certain medications used to induce labor, such as synthetic oxytocin (Pitocin), may cause hyperstimulation of the uterus, leading to excessively frequent or strong contractions that can jeopardize both maternal and fetal well-being.
-
Complications for Preterm Babies: Inducing labor before full term (37 weeks) increases the risk of complications for preterm babies, including respiratory distress syndrome and other neonatal health issues.
- Cervical lacerations or tears due to rapid labor.
METHODS OF INDUCING LABOR
There are several methods used to induce labor, depending on the circumstances and the readiness of the cervix. Here are common methods of inducing labor:
- Ripening of the Cervix: Ripening the cervix involves preparing it for labor by softening and thinning it. This can be done with medications or mechanical methods.
- Synthetic Prostaglandins: Synthetic prostaglandins are hormones that can be administered in the form of tablets inserted into the vagina. Prostaglandins help soften and dilate the cervix, initiating labor.
- Laminaria: Laminaria are slender rods made from seaweed that are inserted into the cervix. As they absorb water, they expand, gradually dilating the cervix and preparing it for labor.
- Balloon Catheter: A small tube with an inflatable balloon on the end is inserted into the cervix and filled with saline solution. The balloon puts pressure on the cervix, causing it to dilate and stimulating the release of natural hormones that initiate labor.
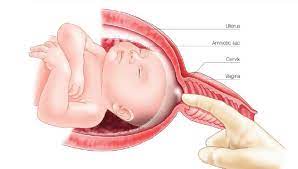
- Membrane Stripping or Sweeping: Membrane stripping, also known as membrane sweeping, involves the healthcare provider inserting a gloved finger into the cervix and separating the amniotic sac from the uterine wall. This can release hormones that help initiate labor.
- Amniotomy (Water Breaking): During an amniotomy, the healthcare provider manually ruptures the amniotic sac using a small plastic hook called an amnihook. This releases amniotic fluid and can help kickstart labor.
- Oxytocin (Pitocin) Infusion: Oxytocin is a hormone that stimulates uterine contractions. It can be administered intravenously to induce or augment labor. The dosage can be adjusted to regulate the strength and frequency of contractions.
- Nipple stimulation: Stimulating the nipples can release oxytocin and may help bring on contractions.
- Herbal Remedies: Some herbal remedies, such as castor oil, black cohosh or evening primrose oil, are believed to have labor-inducing properties. However, their effectiveness and safety are not well-established, these are generally not recommended due to potential risks, and they should only be used under the guidance of a healthcare provider.
CONTRAINDICATIONS TO INDUCING LABOR
There are certain situations in which inducing labor may not be advisable due to potential risks or complications. These contraindications vary depending on the specific circumstances of the pregnancy and the health of the mother and baby. Here are some common contraindications to inducing labor:
- Previous C-section with Classical Incision: Women who have had a previous cesarean section with a classical (vertical) uterine incision may be at increased risk of uterine rupture during labor induction.
- Multiple Previous C-sections: Women who have previous cesarean deliveries may be at increased risk of uterine rupture or other complications during labor induction.
- Placenta Previa: Placenta previa occurs when the placenta partially or completely covers the cervix. Inducing labor in this situation can increase the risk of severe bleeding and other complications.
- Abnormal Fetal Presentation: If the baby is in a breech (buttocks-first) or transverse (sideways) position, inducing labor may not be safe and may increase the risk of birth complications.
- Active Herpes Lesions: Women with active herpes lesions on the vulva may be at increased risk of transmitting the virus to the baby during vaginal delivery. Inducing labor in this situation may not be advisable.
- Umbilical Cord Prolapse: If the umbilical cord slips into the birth canal ahead of the baby (umbilical cord prolapse), inducing labor can compress the cord and compromise blood flow to the baby.
- Cephalopelvic Disproportion (CPD): CPD occurs when the baby’s head is too large to pass safely through the mother’s pelvis. Inducing labor in this situation may increase the risk of prolonged labor, fetal distress, and the need for a cesarean section.
- Triplet or Higher Order Pregnancy: In pregnancies with three or more babies, the risk of complications is higher, and inducing labor may not be safe for both the mother and the babies.
Here are some key precautions to consider:
Medical Evaluation
- Ensure that the decision to induce labor is based on medical necessity (e.g., post-term pregnancy, gestational hypertension, maternal diabetes, or preeclampsia).
- Evaluate the condition of the cervix (cervical ripening) to determine if induction is appropriate. This can be assessed using the Bishop score.
Monitoring
- Continuous fetal monitoring is essential to assess fetal well-being.
- Close monitoring of maternal vital signs, especially for signs of uterine overstimulation, such as excessively frequent or long contractions.
Informed Consent
- Discuss the potential risks, benefits, and alternatives with the mother. Risks of induction include uterine rupture, fetal distress, and increased likelihood of a cesarean section.
Readiness of the Cervix
- The cervix should be assessed for dilation, effacement, and consistency. If the cervix is not ready, induction may be unsuccessful, and the risks may outweigh the benefits.
Timing and Setting
- Labor induction is usually done in a hospital setting where both the mother and fetus can be closely monitored for complications.
- Induction should only be performed when the healthcare provider believes it is medically appropriate and safe.
Avoid Induction Without Medical Indication
- Avoid elective induction before 39 weeks unless there are medical reasons for it, as the baby may not be fully developed before then. Labor induction should be carefully planned and performed under the guidance of experienced healthcare professionals.
Aftercare
- Monitor for complications after induction, including excessive bleeding, infection, or signs of postpartum hemorrhage.
- Ensure adequate pain management and support during labor.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

