What Is Heart Failure? Understanding the Condition and Its Causes
Heart failure (HF), also known as congestive heart failure (CHF), is a serious and potentially life-threatening condition in which the heart is unable to pump enough blood to meet the body’s needs. It occurs when the walls of the heart become too weak or stiff to effectively fill with and pump out sufficient blood throughout the body. Heart failure can be caused by a wide range of factors, such as high blood pressure, coronary artery disease, obesity, diabetes and more. The risk of developing heart failure increases with age and can affect both men and women. Symptoms include shortness of breath, persistent coughing or wheezing, fatigue, swelling of the ankles and feet, rapid or irregular heartbeat, nausea, lack of appetite and more. Treatments include lifestyle changes (i.e., diet modifications), medications to reduce fluid in your body or improve your heart’s pumping strength along with surgically implanted devices like pacemakers or implantable cardioverter-defibrillators (ICDs). With proper treatment and management, patients can live long productive lives despite their diagnosis. Please keep reading for details on the following topics: Please keep reading for details on the following topics:
How the normal heart works
When there is a fault in the normal functioning of the heart
Overview of HF
Causes and types of HF
Risk factors for HF
Symptoms of HF
How heart failure is diagnosed
Complications of HF
How to prevent HF
How HF is managed
Nutritional advice
When to seek urgent medical care
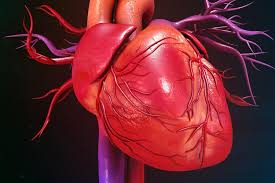
The heart
The heart is a vital organ that circulates oxygen-rich blood throughout the body, supplying nutrients and oxygen to cells and organs while regulating blood pressure and electrolyte balance. Comprising four chambers—two atria and two ventricles—it tirelessly pumps blood, with the left side receiving oxygenated blood from the lungs and delivering it to the body, while the right side receives deoxygenated blood from the body and pumps it to the lungs. This muscular organ, roughly the size of a fist, functions ceaselessly to sustain life.
How the normal heart works
The normal functioning of the heart involves a precise sequence of events to efficiently circulate blood throughout the body:
- Deoxygenated blood returns from the body and enters the right atrium.
- The blood flows into the right ventricle, which then contracts, pumping the blood to the lungs.
- In the lungs, the blood picks up oxygen and releases carbon dioxide, becoming oxygenated.
- Oxygen-rich blood returns to the heart, entering the left atrium.
- From the left atrium, the blood moves into the left ventricle, which contracts forcefully, propelling the oxygenated blood throughout the body.
- This coordinated process ensures that all chambers of the heart work together to maintain circulation and deliver oxygenated blood to tissues and organs.
When there’s a fault in the normal functioning of the heart, several mechanisms attempt to compensate:
- Increased Contractility: The heart may attempt to contract more forcefully to maintain adequate blood flow.
- Hypertrophy: Heart muscle cells may enlarge to increase pumping capacity.
- Tachycardia: The heart may beat faster to pump more blood per unit of time.
- Vasoconstriction: Blood vessels may narrow to maintain blood pressure and redirect blood flow to vital organs.
Causes and types of heart failure

This can be caused by various factors that weaken or damage the heart muscle, impairing its ability to pump blood effectively. The primary causes and types of heart failure include:
- Coronary Artery Disease (CAD): CAD occurs when the arteries supplying blood to the heart become narrowed or blocked due to the buildup of plaque (atherosclerosis). Reduced blood flow to the heart muscle can lead to heart muscle damage and weaken its pumping ability, resulting in heart failure.
- Heart Attack (Myocardial Infarction): A heart attack occurs when blood flow to a part of the heart muscle is blocked, leading to tissue damage or death. This can weaken the heart muscle and contribute to heart failure.
- Hypertension (High Blood Pressure): Chronic high blood pressure can strain the heart, causing it to thicken and become stiffer over time. This increased workload can eventually lead to heart failure.
- Cardiomyopathy: This refers to diseases of the heart muscle, which can be inherited or acquired. Cardiomyopathy can cause the heart muscle to become enlarged, thickened, or rigid, impairing its ability to pump blood effectively and leading to heart failure.
- Valvular Heart Disease: Malfunctioning heart valves, such as aortic stenosis (narrowing of the aortic valve) or mitral regurgitation (leakage of the mitral valve), can disrupt blood flow within the heart, causing it to work harder and potentially leading to heart failure.
- Arrhythmias: Abnormal heart rhythms, such as atrial fibrillation or ventricular tachycardia, can affect the heart’s ability to pump blood efficiently over time, contributing to heart failure.
- Other Factors: Other factors that can contribute to heart failure include diabetes, smoking, obesity, chronic kidney disease, excessive alcohol consumption, certain medications (e.g., nonsteroidal anti-inflammatory drugs, chemotherapy drugs), and infections (e.g., viral myocarditis).
Heart failure can be classified into two main types based on the heart’s pumping ability:
- Systolic Heart Failure: The heart’s ability to contract and pump blood out to the body is impaired, resulting in reduced ejection fraction (the percentage of blood pumped out of the heart with each contraction).
-
Diastolic Heart Failure: The heart’s ability to relax and fill with blood during the resting phase (diastole) is impaired, leading to elevated pressures in the heart chambers and reduced filling capacity. Ejection fraction may be preserved or near-normal in diastolic heart failure.
Several risk factors increase the likelihood of developing heart failure. These include:
- Hypertension (high blood pressure): Chronic high blood pressure can strain the heart muscle, leading to its gradual weakening and eventual heart failure.
- Coronary Artery Disease (CAD): Narrowing or blockage of the coronary arteries reduces blood flow to the heart muscle, increasing the risk of heart failure, especially following a heart attack.
- Previous Heart Attack: A history of myocardial infarction (heart attack) can weaken the heart muscle and predispose individuals to heart failure.
- Cardiomyopathy: Various conditions affecting the heart muscle, such as dilated cardiomyopathy, hypertrophic cardiomyopathy, or restrictive cardiomyopathy, increase the risk of heart failure.
- Valvular Heart Disease: Malfunctioning heart valves, such as aortic stenosis or mitral regurgitation, can disrupt normal blood flow and strain the heart, leading to heart failure.
- Diabetes Mellitus: Diabetes is associated with an increased risk of cardiovascular diseases, including coronary artery disease and hypertension, which contribute to the development of heart failure.
- Obesity: Excess body weight places additional strain on the heart and can lead to conditions such as hypertension, diabetes, and sleep apnea, all of which increase the risk of heart failure.
- Smoking: Cigarette smoking is a significant risk factor for heart disease, including coronary artery disease, atherosclerosis, and heart failure.
- Excessive Alcohol Consumption: Heavy alcohol consumption can weaken the heart muscle (alcoholic cardiomyopathy) and contribute to heart failure.
- Family History: Individuals with a family history of heart failure or other cardiovascular diseases have a higher risk of developing heart failure themselves.
- Age: The risk of heart failure increases with advancing age, particularly in individuals over 65 years old.
- Ethnicity: Certain ethnic groups, such as African Americans, have a higher prevalence of heart failure compared to other populations.
- Gender: Men are at higher risk of developing heart failure at a younger age, while women’s risk increases after menopause.
- Other Medical Conditions: Chronic kidney disease, thyroid disorders, sleep apnea, and certain autoimmune diseases are additional risk factors for heart failure.
Symptoms of heart failure may include:
- Increased tiredness
- Rapid or irregular heartbeat
- Chest pain
- Difficulty breathing, especially with exertion
- Swelling or edema in the abdomen, legs, and ankles
- Fatigue
- Rapid weight gain due to fluid retention
- Continuous coughing or wheezing
- Coughing up white, pink, or foamy mucus
- Difficulty lying flat in bed
- Distended veins in the neck
- Nausea
- Confusion
How heart failure is diagnosed

Diagnosis is conducted through a combination of medical history, physical examination, and various diagnostic tests. The diagnostic process typically includes the following steps:
- Medical History: The healthcare provider will review the patient’s medical history, including symptoms, risk factors, past medical conditions, and family history of heart disease.
- Physical Examination: A thorough physical examination will be conducted to assess signs of heart failure, such as swelling (edema) in the legs or abdomen, abnormal heart sounds, rapid or irregular heartbeat, and signs of fluid buildup in the lungs.
- Diagnostic Tests:
- Blood Tests: Blood tests may be performed to evaluate kidney function, electrolyte levels, liver function, and markers of heart damage (e.g., B-type natriuretic peptide, troponin).
- Imaging Tests: Imaging tests, such as echocardiography (ultrasound of the heart), chest X-ray, or cardiac MRI, may be used to assess the structure and function of the heart, detect abnormalities, and evaluate for signs of fluid buildup in the lungs.
- Electrocardiogram (ECG or EKG): An ECG records the electrical activity of the heart and can help identify abnormal heart rhythms, signs of previous heart attacks, and other cardiac abnormalities.
- Stress Test: A stress test may be performed to evaluate the heart’s response to physical exertion, assess exercise capacity, and detect signs of reduced blood flow to the heart muscle.
- Cardiac Catheterization: In some cases, cardiac catheterization may be performed to assess the coronary arteries’ blood flow and detect blockages or abnormalities.
- Other Tests: Additional tests, such as a Holter monitor (continuous ECG monitoring), CT scan, or nuclear imaging studies, may be ordered based on individual patient factors and suspected underlying causes.
- Assessment of Symptoms: The severity and impact of symptoms, such as shortness of breath, fatigue, and exercise intolerance, are also evaluated as part of the diagnostic process.
-
Evaluation of Ejection Fraction: Ejection fraction, a measure of the heart’s pumping ability, may be assessed through imaging tests such as echocardiography or cardiac MRI. Reduced ejection fraction (typically < 40%) is characteristic of systolic heart failure, while preserved ejection fraction is characteristic of diastolic heart failure.
Complications of heart failure
It can lead to various complications, which may significantly impact a person’s health and quality of life. Some common complications include:
- Kidney Damage or Failure: Decreased blood flow and fluid retention associated with heart failure can impair kidney function, leading to acute kidney injury or chronic kidney disease.
- Arrhythmias: Heart failure can disrupt the heart’s electrical system, increasing the risk of abnormal heart rhythms (arrhythmias), such as atrial fibrillation, ventricular tachycardia, or ventricular fibrillation.
- Heart Valve Problems: Heart failure may lead to dysfunction of heart valves, such as mitral regurgitation or aortic stenosis, further impairing cardiac function and contributing to symptoms.
- Liver Damage: Reduced blood flow and congestion in the liver can lead to liver congestion and impaired liver function, resulting in conditions such as congestive hepatopathy or cirrhosis.
- Pulmonary Hypertension: Elevated pressure in the pulmonary arteries (pulmonary hypertension) can develop as a result of chronic congestion and impaired heart function, leading to further strain on the heart and worsening symptoms.
- Blood Clots: Stagnant blood flow and changes in blood composition associated with heart failure increase the risk of blood clots (thromboembolism), which can lead to complications such as stroke or pulmonary embolism.
- Cardiac Arrest: Severe heart failure can increase the risk of sudden cardiac arrest, a life-threatening condition characterized by the abrupt loss of heart function, leading to loss of consciousness and cessation of breathing.
- Fluid Accumulation in the Lungs (Pulmonary Edema): Fluid buildup in the lungs can lead to pulmonary edema, causing severe shortness of breath, coughing, and wheezing, and potentially leading to respiratory failure.
- Malnutrition: Reduced appetite, gastrointestinal symptoms, and metabolic changes associated with heart failure can lead to malnutrition, further exacerbating weakness and fatigue.
-
Reduced Exercise Tolerance: Progressive muscle weakness, fatigue, and shortness of breath associated with heart failure can impair exercise tolerance and limit physical activity, leading to a further decline in overall health and quality of life.
How to prevent heart failure
This involves adopting a healthy lifestyle and managing underlying medical conditions that increase the risk of heart disease. Here are some key strategies:
- Manage High Blood Pressure: Regularly monitor blood pressure and follow recommendations from healthcare providers to keep it within a healthy range. This may include lifestyle modifications (e.g., healthy diet, regular exercise, weight management) and medication as prescribed.
- Control Cholesterol Levels: Maintain healthy cholesterol levels by following a balanced diet low in saturated and trans fats, engaging in regular physical activity, and taking prescribed medications if necessary.
- Manage Diabetes: Keep blood sugar levels under control through a combination of diet, exercise, medication, and regular monitoring as advised by healthcare providers.
- Maintain a Healthy Weight: Aim for a healthy weight through a balanced diet and regular physical activity. Avoid excessive calorie intake and prioritize nutrient-rich foods.
- Be Physically Active: Engage in regular aerobic exercise (e.g., walking, swimming, cycling) for at least 150 minutes per week, as recommended by healthcare providers. Consult with a healthcare professional before starting any exercise program, especially if you have existing health conditions.
- Eat a Heart-Healthy Diet: Consume a diet rich in fruits, vegetables, whole grains, lean protein sources, and healthy fats. Limit intake of processed foods, sugary beverages, and foods high in saturated and trans fats, cholesterol, and sodium.
- Quit Smoking: If you smoke, quit smoking to reduce the risk of heart disease and other health complications. Seek support from healthcare providers, smoking cessation programs, or support groups to help you quit successfully.
- Limit Alcohol Consumption: Drink alcohol in moderation or avoid it altogether, as excessive alcohol consumption can contribute to heart disease and increase the risk of heart failure.
- Manage Stress: Practice stress-reducing techniques such as meditation, deep breathing exercises, yoga, or engaging in hobbies and activities you enjoy.
- Get Regular Health Check-ups: Schedule regular check-ups with healthcare providers to monitor your overall health, assess risk factors for heart disease, and address any concerns or symptoms promptly.
- Adhere to Medication Regimens: Take prescribed medications as directed by healthcare providers to manage underlying medical conditions such as high blood pressure, diabetes, and high cholesterol.
-
Know Your Family History: Be aware of your family history of heart disease and discuss it with healthcare providers. Understanding your genetic predispositions can help tailor preventive measures and screening recommendations.
How heart failure is managed
Management involves a comprehensive approach aimed at reducing symptoms, improving quality of life, and preventing complications. Here are some key components:
- Medication Therapy:
- Medications are prescribed to improve heart function, reduce symptoms, and prevent complications. These may include:
- ACE inhibitors or ARBs: To improve the heart’s ability to pump blood and reduce blood pressure.
- Beta-blockers: To slow the heart rate, reduce strain on the heart, and improve heart function.
- Diuretics: To remove excess fluid from the body and reduce swelling (edema).
- Aldosterone antagonists: To reduce fluid retention and improve heart function.
- Anticoagulants: To prevent blood clots and reduce the risk of stroke.
- Statins: To lower cholesterol levels and reduce the risk of cardiovascular events.
- Medications are prescribed to improve heart function, reduce symptoms, and prevent complications. These may include:
- Dietary Changes:
- Sodium restriction: Limiting sodium intake helps reduce fluid retention and swelling.
- Fluid restriction: Limiting fluid intake helps prevent fluid overload and congestion in the body.
- Following a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins can also support overall cardiovascular health.
- Lifestyle Modifications:
- Regular physical activity: Engaging in appropriate exercise under the guidance of healthcare professionals can improve heart function, endurance, and overall well-being.
- Smoking cessation: Quitting smoking reduces the risk of cardiovascular complications and improves overall health.
- Limiting alcohol consumption: Moderating alcohol intake or avoiding it altogether can help manage heart failure symptoms and reduce the risk of complications.
- Monitoring and Self-care:
- Regular monitoring of weight, blood pressure, and symptoms helps detect changes early and adjust treatment accordingly.
- Adhering to medication regimens and following healthcare provider recommendations is essential for managing heart failure effectively.
- Educating oneself about heart failure, its symptoms, and management strategies empowers individuals to take an active role in their care.
- Surgical Interventions:
- In some cases, surgical procedures may be necessary to manage heart failure, such as:
- Coronary artery bypass surgery: To improve blood flow to the heart muscle.
- Heart valve repair or replacement: To address valvular heart disease.
- Implantation of a pacemaker or defibrillator: To regulate heart rhythm and prevent arrhythmias.
- Heart transplant: For severe cases of heart failure when other treatments are ineffective.
- In some cases, surgical procedures may be necessary to manage heart failure, such as:
-
Management of Comorbidities:
- Managing underlying conditions such as hypertension, diabetes, and obesity is essential for overall heart failure management and improving outcomes.
Nutritional advice
Nutritional advice plays a crucial role in managing heart failure and promoting overall cardiovascular health. Here are some key dietary recommendations:
- Ensure Healthy Foods:
- Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins. These foods provide essential nutrients, vitamins, and minerals necessary for heart health.
- Eat Foods Rich in Fiber:
- Incorporate fiber-rich foods such as whole grains, fruits, vegetables, legumes, and nuts into your diet. Fiber helps regulate digestion, lower cholesterol levels, and maintain a healthy weight.
- Avoid Fatty and Sugary Foods:
- Limit consumption of foods high in saturated and trans fats, as well as sugary snacks and beverages. These can contribute to weight gain, high cholesterol levels, and increased risk of cardiovascular disease.
- Choose Low-Fat and Fat-Free Foods:
- Opt for lean protein sources such as skinless poultry, fish, beans, and legumes. Choose low-fat or fat-free dairy products to reduce intake of saturated fat.
- Limit Salt Intake:
- Reduce the amount of salt (sodium) in your diet by avoiding processed and packaged foods, which often contain high levels of sodium. Use herbs, spices, and other flavorings to season foods instead of salt.
- Avoid Alcohol:
- Limit or avoid alcohol consumption, as it can worsen heart failure symptoms and interact with medications. Alcohol can also contribute to dehydration and heart rhythm disturbances.
- Limit Foods High in Cholesterol:
- Limit intake of foods high in cholesterol, such as fatty meats, egg yolks, and full-fat dairy products. Choose lean protein sources and low-fat dairy alternatives instead.
- Monitor Fluid Intake:
- Keep track of your fluid intake, including water, soups, and beverages. Follow any fluid restrictions prescribed by your healthcare provider to prevent fluid overload and swelling (edema).
- Practice Portion Control:
- Pay attention to portion sizes and avoid overeating. Eating smaller, more frequent meals throughout the day can help prevent bloating and discomfort.
-
Seek Nutritional Guidance:
- Consult with a registered dietitian or nutritionist specializing in heart-healthy diets for personalized dietary recommendations and meal planning strategies tailored to your individual needs and preferences.
When to seek urgent medical care
Knowing when to seek urgent medical care for heart failure is crucial for managing the condition and preventing serious complications. Here are some signs and symptoms that indicate the need for immediate medical attention:
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

