From Bunions to Plantar Fasciitis: Solutions for Common Foot Problems
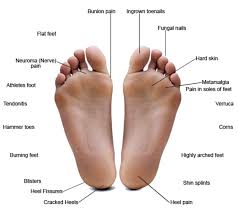
Foot problems can affect people of all ages and can be caused by a variety of factors, including injury, disease, and genetic predisposition. Proper foot care, including regular washing, nail trimming, and wearing appropriate footwear, can help prevent foot problems and promote overall foot health. Foot problems are common and can range from minor issues such as blisters and corns to more serious conditions such as plantar fasciitis, bunions, and neuropathy. We will address the following topics:
Causes of foot problems
Blisters
Plantar fasciitis
Heel pain
Achilles tendonitis
Bunions
Hammer toes
Flat feet
Neuropathy
Ingrown toenails
Plantar warts
Foot pain
Heel pain
Claw Toes and Mallet Toes
Gout
Stress fractures
Natural remedies to resolve foot problems
How to buy proper fitting shoes
Magnets and foot problems
Overview of the foot
The foot is an anatomical structure that is part of the lower limb and is essential for standing, walking, and running. It consists of 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments. The foot is divided into three sections: the hindfoot, the midfoot, and the forefoot. The hind foot consists of the heel bone (calcaneus) and the ankle bone (talus), which work together to provide stability and support. The midfoot includes five tarsal bones that form the arch of the foot and provide shock absorption. The forefoot consists of the metatarsal bones and the toes (phalanges) and is responsible for propulsion and balance during walking and running. The foot is designed to distribute weight evenly across the entire foot, absorb shock, and provide stability and flexibility. The arch of the foot is particularly important for shock absorption and weight distribution. The foot also contains numerous sensory receptors that provide information about the surface and terrain to the brain, which is important for balance and coordination.
Causes of foot problems
There are many different causes of foot problems, including:
- Improper footwear: Wearing shoes that do not fit properly or lack adequate support can lead to a variety of foot problems, including blisters, calluses, corns, and even more serious issues such as plantar fasciitis or stress fractures.
- Overuse injuries: Engaging in activities that involve repetitive motion, or high impact can lead to overuse injuries, such as Achilles tendonitis, plantar fasciitis, or stress fractures.
- Trauma: Foot injuries resulting from accidents, falls, or other traumas can cause a range of problems, including sprains, fractures, and dislocations.
- Medical conditions: Certain medical conditions can affect the health of your feet, such as diabetes, arthritis, and peripheral artery disease.
- Genetics: Some foot problems can be inherited, such as flat feet or high arches, which can lead to issues like plantar fasciitis or bunions.
- Aging: As we age, our feet can become more prone to issues such as arthritis, joint pain, and reduced circulation.
- Poor posture or alignment: Poor posture or alignment can put extra pressure on certain parts of the foot, leading to issues like bunions or hammertoes.
Here are some common foot problems:
- Blisters: Blisters are fluid-filled pockets that develop on the skin, usually caused by friction or pressure.
- Corns and calluses: Corns and calluses are areas of thickened skin that form on the feet due to pressure or friction.
- Plantar fasciitis: Plantar fasciitis is a condition in which the plantar fascia, a band of tissue that runs along the bottom of the foot, becomes inflamed and painful.
- Bunions: A bunion is a bony bump that forms on the joint at the base of the big toe. It can be painful and make it difficult to wear shoes.
- Neuropathy: Neuropathy is a condition in which the nerves that supply the feet are damaged, causing pain, numbness, and tingling.
- Ingrown toenails: An ingrown toenail occurs when the nail grows into the skin, causing pain, redness, and swelling.
- Athlete’s foot: Athlete’s foot is a fungal infection that affects the skin on the feet, causing itching, burning, and peeling.
- Plantar warts: Plantar warts are small growths that appear on the soles of the feet and are caused by a virus.
- Foot odor
Blisters

Blisters are fluid-filled sacs that form on the surface of the skin. They can be caused by a variety of factors, including friction, pressure, burns, and exposure to irritants. Blisters on the foot are a common problem, often caused by friction or rubbing from ill-fitting shoes, socks, or another footwear. Here are some tips to help prevent blisters on the foot:
- Wear properly fitting shoes: Shoes that are too tight or too loose can cause friction and lead to blisters. Choose shoes that fit well and provide enough room for your toes to move freely.
- Wear moisture-wicking socks: Moisture can increase the risk of blisters, so choose socks made from materials that wick away sweat and moisture, such as synthetic blends or wool.
- Use blister pads or moleskin: If you know you’re prone to blisters, consider using a blister pad or moleskin to protect your feet from friction.
- Break in new shoes gradually: If you’ve recently purchased a new pair of shoes, wear them for short periods of time at first and gradually increase the duration to allow your feet to adjust.
- Keep your feet dry: Moisture can increase the risk of blisters, so make sure to dry your feet thoroughly after showering or swimming.
Corns and calluses are areas of thickened skin that form on the feet due to pressure or friction.
Plantar fasciitis

Plantar fasciitis is a condition in which the plantar fascia, a band of tissue that runs along the bottom of the foot, becomes inflamed and painful. In other words, plantar fasciitis causes pain in the heel and bottom of the foot. It is caused by inflammation of the plantar fascia, a thick band of tissue that connects the heel bone to the toes.
Symptoms of plantar fasciitis
Pain in the heel, which is often worst in the morning or after periods of rest
The pain may also be triggered by activities such as running, walking, or standing for long periods of time.
Causes of plantar fasciitis
- Overuse or repetitive strain: Activities that put a lot of stress on the feet, such as running, exercising or playing sports can lead to plantar fasciitis.
- Foot structure: People with flat feet, high arches, or an abnormal gait or uneven stride that puts pressure on the foot causing one to be prone to plantar fasciitis.
- Obesity: Being overweight can put extra pressure on the feet and increase the risk of plantar fasciitis.
- Age: Plantar fasciitis is more common in people over 40.
- Improper footwear: Wearing shoes that don’t provide enough support, or cushioning can increase the risk of plantar fasciitis.
Treatment for plantar fasciitis typically involves a combination of rest, stretching exercises, and supportive footwear. Your healthcare provider may also recommend orthotics or shoe inserts, physical therapy, or in some cases, surgery. It’s important to seek medical attention if you’re experiencing symptoms of plantar fasciitis, as early treatment can help prevent the condition from getting worse.
Heel pain

This can be caused by a variety of factors, including plantar fasciitis, Achilles tendonitis, heel spurs, or a stress fracture. Here are some tips to help decrease heel pain:
- Rest: Avoid activities that exacerbate your heel pain and take a break from any high-impact exercises, such as running or jumping.
- Stretching: Gentle stretching exercises can help loosen the muscles and tissues in the foot, reducing tension and pain. Try calf stretches and plantar fascia stretches.
- Ice: Applying ice to the affected area can help reduce inflammation and relieve pain. Use an ice pack or frozen water bottle for 15-20 minutes at a time, several times a day.
- Supportive footwear: Wearing shoes with good arch support and cushioning can help reduce the impact on your feet and decrease heel pain. Avoid high heels and flip-flops, which can exacerbate heel pain.
- Over-the-counter pain relievers: Over-the-counter pain medications such as ibuprofen or acetaminophen can help alleviate pain and reduce inflammation.
- Physical therapy: A physical therapist can work with you to develop an exercise program that helps to stretch and strengthen the muscles and tissues in your feet and lower legs.
Stretches to decrease heel pain
Stretching exercises can help reduce heel pain by loosening the muscles and tissues in the foot, reducing tension and inflammation. Here are some stretching exercises that may help decrease heel pain:
- Calf stretch: Stand facing a wall with your hands on the wall at shoulder height. Step one foot back and press the heel of that foot down towards the ground, keeping the knee of the other leg bent. Hold for 15-30 seconds and then switch legs.
- Plantar fasciae stretch: Sit in a chair and cross one leg over the other. Using your hand, pull the toes of the crossed foot back towards your shin until you feel a stretch in the arch of your foot. Hold for 15-30 seconds and then switch legs.
- Achilles tendons stretch: Stand facing a wall with your hands on the wall at shoulder height. Step one foot back and keep the back leg straight, pressing the heel towards the ground. Hold for 15-30 seconds and then switch legs.
- Toe stretch: Sit in a chair and place one foot on the opposite thigh. Using your hand, gently stretch each toe back and forth, holding each stretch for a few seconds.
- Ankle rolls: Sit in a chair and lift one foot off the ground. Rotate the ankle in a circular motion, first in one direction and then in the other. Repeat for 10-15 rotations and then switch legs.
Achilles tendonitis

Achilles tendonitis is a condition that causes pain, inflammation, and stiffness in the Achilles tendon, which is the large tendon that connects the calf muscles to the heel bone.
Symptoms of Achilles tendonitis
The main symptoms of Achilles tendonitis are pain and stiffness in the Achilles tendon, which is often worst in the morning or after periods of rest.
The area around the tendon may also be tender or swollen.
Causes of Achilles tendonitis
Achilles tendonitis can be caused by a variety of factors, including:
- Overuse or repetitive strain: Activities that put a lot of stress on the Achilles tendon, such as running or jumping, can lead to Achilles tendonitis.
- Tight calf muscles: If the calf muscles are tight, they can put extra strain on the Achilles tendon, leading to inflammation and pain.
- Improper footwear: Wearing shoes that don’t provide enough support, or cushioning can increase the risk of Achilles tendonitis.
- Age: Achilles tendonitis is more common in people over 40.
- Buildup of cholesterol
Treatment for Achilles tendonitis typically involves a combination of rest, stretching exercises, and supportive footwear. Your healthcare provider may also recommend orthotics or shoe inserts, physical therapy, or in some cases, surgery.
Here are some tips for managing Achilles tendonitis:
- Rest: Avoid activities that exacerbate your Achilles tendon pain and take a break from any high-impact exercises, such as running or jumping.
- Stretching: Gentle stretching exercises can help loosen the muscles and tissues in the calf and reduce tension on the Achilles tendon.
- Ice: Applying ice to the affected area can help reduce inflammation and relieve pain. Use an ice pack or frozen water bottle for 15-20 minutes at a time, several times a day.
- Supportive footwear: Wearing shoes with good arch support and cushioning can help reduce the impact on your feet and decrease Achilles tendon pain.
- Over-the-counter pain relievers: Over-the-counter pain medications such as ibuprofen or acetaminophen can help alleviate pain and reduce inflammation.
It’s important to seek medical attention if your Achilles tendonitis persists or worsens, as your healthcare provider may recommend additional treatment options, such as custom orthotics or corticosteroid injections.
Cholesterol and the Achilles tendon
There is some evidence to suggest that a buildup of cholesterol in the arteries may increase the risk of developing Achilles tendonitis. Cholesterol is a waxy substance that can accumulate in the walls of arteries, leading to the formation of plaques. Over time, these plaques can narrow the arteries, reducing blood flow to the tissues and organs.
The Achilles tendon, like other tendons and ligaments in the body, requires a good blood supply to remain healthy and function properly. If the blood flow to the Achilles tendon is reduced due to a buildup of cholesterol in the arteries, it may become more prone to injury and inflammation. In addition, high levels of cholesterol in the blood can contribute to the development of other health conditions, such as obesity and diabetes, which can also increase the risk of Achilles tendonitis.
To reduce the risk of developing Achilles tendonitis and other health problems associated with high cholesterol, it’s important to maintain a healthy lifestyle. This includes:
- Eating a balanced diet that is low in saturated and trans fats, and high in fruits, vegetables, and whole grains.
- Getting regular exercise, including stretching and strengthening exercises that can help prevent injury.
- Maintaining a healthy weight.
- Managing any underlying health conditions, such as diabetes or high blood pressure, that may contribute to the buildup of cholesterol in the arteries.
- Avoiding smoking and limiting alcohol consumption.
If you are experiencing Achilles tendonitis or other symptoms that may be related to high cholesterol, it’s important to speak with your healthcare provider. They can recommend appropriate treatment options, such as medications to lower cholesterol levels or lifestyle changes to help reduce your risk of developing further health complications.
Bunions

Bunions are bony bumps that develop on the joint at the base of the big toe. They occur when the bones in the front part of the foot move out of place, causing the big toe to lean toward the other toes instead of pointing straight ahead. This shift in position can cause the joint at the base of the big toe to become enlarged and inflamed, resulting in a bunion. This can be painful and make it difficult to wear shoes.
Some of the common causes of bunions include:
- Genetics: Bunions can run in families, so if you have a family history of bunions, you may be more likely to develop them.
- Footwear: Tight, narrow shoes that squeeze the toes together can put pressure on the joints of the foot and increase the risk of developing bunions.
- Foot structure: People with certain foot structures, such as flat feet or a high arch, may be more susceptible to developing bunions.
-
Arthritis: Certain types of arthritis can cause inflammation in the joints of the foot, which can increase the likelihood of developing bunions.
Symptoms of a bunion
The main symptom of a bunion is a visible bump on the side of the foot, near the base of the big toe.
Other symptoms may include pain, swelling, and redness in the affected area, as well as difficulty walking or finding comfortable footwear.
Treatment options for bunions may include:
- Footwear modifications: Wearing shoes that are wider and have a larger toe box can help relieve pressure on the bunion and reduce pain.
- Padding and taping: Placing pads or moleskin on the bunion, or taping the affected toe, can help protect the area and reduce pain.
- Orthotics: Custom-made shoe inserts can help redistribute pressure on the foot and relieve pain.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and reduce inflammation.
- Surgery: In severe cases, surgery may be necessary to realign the bones in the foot and remove the bunion.
Claw Toes and Mallet Toes
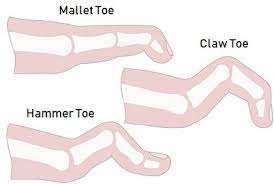
Claw toes and mallet toes are both foot deformities that involve the toes. In both cases, the toes bend abnormally and can become painful over time.
Claw toes are a condition in which the toes bend upward from the joint at the ball of the foot and then downward at the middle joint, giving the appearance of a claw. This deformity can be caused by nerve damage or muscle weakness in the foot. It can also be caused by wearing ill-fitting shoes that force the toes into a bent position over a long period of time.
Mallet toes, on the other hand, occur when the joint at the end of the toe (the distal interphalangeal joint) bends downward, causing the tip of the toe to point downward as well. This condition is often caused by wearing shoes that are too tight or too narrow in the toe box.
Both claw toes and mallet toes can cause discomfort, pain, and difficulty with walking. Treatment options include wearing properly fitted shoes with adequate room in the toe box, orthotics, splints, and in severe cases, surgery. It is important to seek medical attention if you are experiencing foot pain or notice a change in the shape of your toes.

Toenail fungus, also known as onychomycosis, is a common fungal infection that affects the nails of the toes. The infection typically begins as a white or yellow spot under the tip of the toenail and can spread deeper into the nail over time.
Toenail fungus is caused by a group of fungi called dermatophytes but can also be caused by other types of fungi or yeast. The fungus thrives in warm, moist environments and can be spread through contact with infected skin or nail clippings.
Symptoms of toenail fungus can include thickened or brittle nails, a distorted shape, a foul odor, and a yellow, brown, or white discoloration. The infection can be uncomfortable or painful and may interfere with daily activities.
Treatment options for toenail fungus include topical antifungal creams or nail lacquers, oral antifungal medications, and laser therapy. It is important to continue treatment until the infection is completely cleared, which may take several months. Preventative measures such as keeping feet clean and dry, wearing breathable shoes and socks, and avoiding shared nail clippers or other pedicure tools can also help prevent toenail fungus.

Diabetic foot refers to a range of foot problems that can occur in people with diabetes. Diabetes can cause damage to the nerves and blood vessels in the feet, which can lead to poor circulation and reduced sensitivity to pain. This can make it difficult to notice foot injuries, such as blisters, cuts, or sores, which can then lead to serious complications.
Some common foot problems associated with diabetes include peripheral neuropathy, which causes tingling, numbness, or pain in the feet, as well as peripheral artery disease, which can cause poor circulation and slow healing of foot injuries. Other foot problems can include calluses, corns, fungal infections, and foot ulcers.
Preventing and managing diabetic foot requires good blood sugar control and regular foot care. People with diabetes should inspect their feet daily for cuts, sores, or other signs of injury, and should seek medical attention if they notice any changes in their feet. They should also wear well-fitting shoes and socks and avoid going barefoot. Regular visits to a healthcare provider or foot specialist are also important for monitoring and managing foot health.
Hammer toes

Hammer toes are a common foot condition in which the middle joint of a toe becomes bent, causing the toe to curl downward. This can occur in any of the toes, but it most commonly affects the second or third toe. Hammer toes can cause discomfort, pain, and difficulty with walking or wearing shoes.
Causes of hammer
The main causes of hammer toes include:
- Tight shoes: Shoes that are too tight or narrow can force the toes into a cramped position and increase the risk of developing hammer toes.
- Foot structure: People with certain foot structures, such as flat feet or a high arch, may be more susceptible to developing hammer toes.
- Trauma: Injuries to the toe, such as stubbing or breaking it, can cause the toe to become misaligned and increase the risk of developing hammer toes.
-
Genetics: Hammer toes can run in families, so if you have a family history of the condition, you may be more likely to develop it.
Treatment options for hammer toes may include:
- Footwear modifications: Wearing shoes that have a larger toe box and are not too tight can help relieve pressure on the toes and prevent the condition from worsening.
- Toe exercises and stretches: Exercises and stretches that target the toes and feet can help improve flexibility and reduce pain.
- Padding and taping: Placing pads or moleskin on the affected toe, or taping the toe to the adjacent toe, can help protect the area and reduce pain.
- Orthotics: Custom-made shoe inserts can help redistribute pressure on the foot and relieve pain.
- Surgery: In severe cases, surgery may be necessary to realign the affected toe and alleviate pain.
If you suspect you have hammer toes, it’s important to seek medical attention. Your healthcare provider can help diagnose the condition and recommend appropriate treatment options based on the severity of your symptoms.
Flat feet
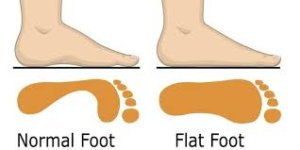
Flat feet, also known as fallen arches, is a condition where the arch of the foot collapses or flattens, causing the entire sole of the foot to come into contact with the ground when standing. This can cause discomfort, pain, and difficulty with walking or standing for long periods.
Flat feet can be caused by a number of factors, including:
- Genetics: Flat feet can be inherited, so if someone in your family has the condition, you may be more likely to develop it.
- Weak arches: Weak muscles and tendons in the feet and legs can cause the arches to collapse.
- Injury or trauma: Injuries or trauma to the foot or ankle can cause flat feet.
- Aging: As we age, the tendons and ligaments in our feet may weaken, causing the arches to collapse.
- Certain medical conditions: Certain medical conditions, such as arthritis, can cause flat feet.
The main symptoms of flat feet may include:
- Pain or discomfort in the feet, especially in the arch or heel.
- Swelling or inflammation in the feet.
- Fatigue or weakness in the feet or legs.
- Difficulty standing or walking for long periods.
Treatment options for flat feet may include:
- Footwear modifications: Wearing shoes that provide good arch support and cushioning can help alleviate pain and discomfort.
- Orthotics: Custom-made shoe inserts or arch supports can help support the arches and relieve pain.
- Physical therapy: Exercises and stretches that target the feet and legs can help improve strength and flexibility and reduce pain.
- Medications: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help alleviate pain and reduce inflammation.
- Surgery: In severe cases, surgery may be necessary to reconstruct the arch and alleviate pain.
How to check for flat feet
You can check for flat feet by performing a simple at-home test called the “wet foot test”. Here’s how to do it:
- Wet the bottom of your foot or dip it in water.
- Step onto a piece of paper or a flat surface that will leave a clear footprint.
- Step off the paper and examine the footprint.
If you have normal arches, you should see an inward curve in the middle of the foot that connects the ball of the foot to the heel. If you have flat feet, the footprint will show the entire sole of the foot, with little to no curve in the middle.
It’s important to note that the wet foot test is not a definitive diagnosis for flat feet. If you suspect you have flat feet or are experiencing any foot pain or discomfort, it’s important to seek medical attention. Your healthcare provider can help diagnose the condition and recommend appropriate treatment options based on the severity of your symptoms.
Neuropathy

Neuropathy is a condition that occurs when there is damage or dysfunction of the nerves in the body, typically in the peripheral nervous system, which includes nerves outside the brain and spinal cord. This can result in a range of symptoms, including pain, numbness, tingling, or weakness in the affected area. There are many different types of neuropathies, each with its own set of causes and symptoms.
Some common causes of neuropathy include:
- Diabetes: Diabetes is one of the most common causes of neuropathy. High blood sugar levels can damage the nerves over time.
- Alcoholism: Long-term heavy alcohol use can also cause neuropathy.
- Autoimmune diseases: Certain autoimmune diseases, such as lupus or rheumatoid arthritis, can cause neuropathy.
- Vitamin deficiencies: Deficiencies in certain vitamins, such as B vitamins, can cause nerve damage.
- Trauma: Injuries that damage the nerves can cause neuropathy.
Treatment options for neuropathy depend on the underlying cause and the severity of the symptoms. In some cases, treating the underlying condition can help alleviate neuropathy symptoms. Other treatment options may include:
- Medications: There are a variety of medications that can be used to treat neuropathy, including pain relievers, anticonvulsants, and antidepressants.
- Physical therapy: Exercises and stretches that target the affected area can help improve strength and flexibility and reduce pain.
- Transcutaneous electrical nerve stimulation (TENS): This involves placing electrodes on the skin that deliver electrical impulses to the affected area, which can help alleviate pain.
- Surgery: In severe cases, surgery may be necessary to repair nerve damage or alleviate pressure on the nerves.
Ingrown toenails

Ingrown toenails occur when the corner or side of a toenail grows into the skin, causing pain, redness, swelling, and sometimes infection. This condition can be caused by a number of factors, including:
- Incorrect nail trimming: Cutting the toenail too short or rounding the edges can cause the nail to grow into the skin.
- Tight shoes: Wearing shoes that are too tight or too small can put pressure on the toenails and cause them to grow abnormally.
- Genetics: Some people are more prone to developing ingrown toenails due to the shape of their toes or the way their nails grow.
- Trauma: Injuries to the toe or toenail can cause the nail to grow abnormally and become ingrown.
To prevent ingrown toenails, it’s important to wear comfortable shoes that fit well and to trim your toenails straight across, without rounding the edges. If you do develop an ingrown toenail, there are several at-home remedies that may help, including soaking your foot in warm water, gently pushing the skin away from the nail with a cotton ball or dental floss, and applying an over-the-counter antiseptic ointment. In more severe cases, your healthcare provider may need to remove the ingrown portion of the toenail or prescribe antibiotics to treat any infection. If you have diabetes or another condition that affects circulation, it’s important to seek medical attention for ingrown toenails to prevent complications.
Plantar warts

Plantar warts are small growths that appear on the soles of the feet. They are caused by the human papillomavirus (HPV) and can be spread through direct contact with an infected person or by walking barefoot in moist areas like public swimming pools or locker rooms.
Plantar warts can be recognized by their thick, rough, and often callused appearance. They may also have small black dots, which are actually blood vessels that have grown into the wart.
Treatment options for plantar warts depend on the severity of the warts and the patient’s preference. Some common treatments include:
- Over-the-counter remedies: There are several over-the-counter wart removal products that can be applied directly to the wart, such as salicylic acid or cryotherapy agents.
- Prescription medications: In some cases, prescription medications, such as bleomycin, can be used to treat plantar warts.
- Surgical removal: For more severe or persistent warts, your healthcare provider may need to remove the wart surgically or with a laser.
- Immunotherapy: This involves stimulating the immune system to fight the virus that causes warts.
It’s important to note that plantar warts can be difficult to treat and may take several weeks or months to resolve. It’s also important to take steps to prevent the spread of plantar warts, such as wearing shoes in public areas and avoiding direct contact with an infected person. If you suspect you have plantar warts or are experiencing any foot pain or discomfort, it’s important to seek medical attention.
Foot pain

Foot pain can be caused by a variety of factors, ranging from overuse to injury or a medical condition. Some common causes of foot pain include:
- Plantar fasciitis: This is a condition that causes pain in the heel and bottom of the foot, usually caused by overuse or repetitive stress on the foot.
- Achilles tendonitis: This is a condition that causes pain in the back of the heel, usually caused by overuse or injury to the Achilles tendon.
- Bunions: This is a deformity of the big toe joint that can cause pain and swelling in the foot.
- Neuropathy: This is a condition that causes damage to the nerves in the feet and can cause pain, numbness, or tingling sensations.
- Flat feet: This is a condition in which the arches of the feet collapse, causing pain and discomfort.
- Gout: This is a type of arthritis that causes sudden, severe pain and swelling in the joints, including the feet.
- Stress fractures: These are small cracks in the bones of the feet, usually caused by overuse or repetitive stress.
- Natural changes in the foot’s size and shape
- High impact exercise
- Poor posture
- Wearing ill-fitting shoes

Gout is often associated with a diet high in purines, a substance found in many foods such as red meat, seafood, and alcohol. Certain medications and medical conditions, such as high blood pressure and kidney disease, can also increase the risk of developing gout.
Treatment for gout usually involves medications to reduce pain and inflammation, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and colchicine. Lifestyle changes, such as reducing purine-rich foods and alcohol intake, can also help prevent gout attacks. Your healthcare provider may also recommend medications to reduce uric acid levels in the blood, such as allopurinol.
If you are experiencing sudden, severe joint pain and swelling, especially in the big toe, it’s important to seek medical attention to determine if it may be gout or another condition. With proper treatment and lifestyle changes, gout can be managed and prevented from causing further damage to the joints.
Foot odor

Foot odor is a common problem that can be caused by a buildup of sweat and bacteria on the skin of the feet. There are several steps you can take to help reduce foot odor, including:
- Practice good hygiene: Wash your feet with soap and water regularly, especially after exercise or other physical activity. Dry your feet thoroughly, especially between the toes.
- Wear breathable shoes: Choose shoes made from breathable materials, such as leather or mesh, that allow air to circulate around your feet.
- Wear moisture-wicking socks: Choose socks made from synthetic materials that help wick moisture away from the skin, such as nylon or polyester especially when exercising.
- Use foot powder: Apply foot powder to your feet and inside your shoes to help absorb moisture and reduce odor.
- Change your shoes and socks regularly: Alternate your shoes and socks every day to allow them to dry out completely between wearings.
- Use antiperspirant: Apply antiperspirant to the soles of your feet to help reduce sweating.
- Soak your feet: Soaking your feet in a solution of warm water and vinegar or Epsom salt can help kill bacteria and reduce odor.
Natural remedies to resolve foot problems
There are several natural remedies that may help to alleviate foot problems, although it’s important to note that the effectiveness of these remedies may vary depending on the individual and the specific foot problem. It’s important to note that these natural remedies are not a substitute for medical treatment, and if you are experiencing foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs. Here are some natural remedies that may be helpful:
Epsom salt soak

Epsom salt contains magnesium, which can help to relax muscles and reduce swelling. Epsom salt is a popular natural remedy for foot problems due to its ability to reduce inflammation and relieve pain. Epsom salt is a mineral compound that contains magnesium and sulfate, and when dissolved in water, it is easily absorbed through the skin.
Soaking your feet in warm water mixed with Epsom salt may be helpful for a variety of foot problems, including plantar fasciitis, heel pain, and swollen or tired feet. Epsom salt can help to reduce inflammation and relax muscles, which can help to alleviate pain and promote healing.
To use Epsom salt for foot problems, dissolve 1/2 to 1 cup of Epsom salt in a basin of warm water and soak your feet for 15-20 minutes. You can repeat this process once or twice a day, as needed.
Essential oils

Essential oils can be a natural and effective way to help alleviate foot problems. Dilute a few drops of essential oil in a carrier oil, such as coconut oil, and massage into the affected area. Some essential oils have anti-inflammatory, pain-relieving, and antimicrobial properties that can help to reduce pain, swelling, and infection.
Here are some essential oils that may be helpful for different foot problems:
- Tea tree oil: is a natural antimicrobial and antifungal agent that can be helpful for toenail fungus and athlete’s foot. Dilute a few drops of tea tree oil in a carrier oil and apply it directly to the affected area.
- Peppermint oil: has a cooling effect and can help to relieve pain and inflammation. Dilute a few drops of peppermint oil in a carrier oil and massage it into the affected area.
- Lavender oil: has anti-inflammatory and pain-relieving properties and can be helpful for foot pain, including plantar fasciitis. Dilute a few drops of lavender oil in a carrier oil and massage it into the affected area.
- Eucalyptus oil: has anti-inflammatory and pain-relieving properties and can be helpful for foot pain, including arthritis and neuropathy. Dilute a few drops of eucalyptus oil in a carrier oil and massage it into the affected area.
It’s important to note that essential oils should always be diluted in a carrier oil before applying to the skin, as they can be irritating or even harmful if used undiluted. It’s also important to test a small area of skin before using a new essential oil to make sure you don’t have an allergic reaction.
While essential oils can be a helpful natural remedy for foot problems, they are not a substitute for medical treatment. If you are experiencing foot pain or other foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Ice therapy

Ice therapy, also known as cryotherapy, is a simple and effective natural remedy for foot problems such as plantar fasciitis, heel pain, and other types of foot pain. Ice therapy can help to reduce inflammation, numb pain, and promote healing.
To use ice therapy for foot problems, you can either use an ice pack or make your own by wrapping ice in a towel or a plastic bag. Apply the ice pack to the affected area for 15-20 minutes at a time, several times a day. It’s important to avoid applying ice directly to the skin, as this can cause frostbite or damage to the skin.
Alternatively, you can use a frozen water bottle to massage your foot by rolling it back and forth under your foot. This can help to relieve pain and inflammation, as well as stretch the plantar fascia.
Ice therapy is most effective when used in combination with other treatments such as stretching, rest, and proper footwear. It’s important to note that ice therapy is not a substitute for medical treatment, and if you are experiencing foot pain or other foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Exercise and stretching

Exercise and stretching can be very beneficial for foot problems, including plantar fasciitis, Achilles tendonitis, flat feet, and many others. Regular exercise and stretching can help to strengthen the muscles and ligaments in your feet and toes, improve flexibility, and reduce the risk of injury.
Here are some exercises and stretches that can be helpful for foot problems:
- Calf stretches: Tight calf muscles can contribute to many foot problems, including plantar fasciitis and Achilles tendonitis. To stretch your calves, stand facing a wall with one foot forward and one foot back, keeping both heels on the ground. Lean forward towards the wall, keeping your back leg straight, until you feel a stretch in your calf. Hold for 20-30 seconds and repeat on the other side.
- Toe curls: can help to strengthen the muscles in your feet and improve flexibility. Sit in a chair with your feet flat on the ground. Curl your toes under your foot and then release them. Repeat 10-15 times.
- Arch stretches: can help to stretch the plantar fascia, which can be helpful for plantar fasciitis. Sit in a chair with one foot on the opposite knee. Gently pull your toes back towards your shin until you feel a stretch in the arch of your foot. Hold for 20-30 seconds and repeat on the other side.
- Ankle circles: can help to improve flexibility in your ankle and reduce the risk of ankle sprains. Sit in a chair with your feet flat on the ground. Lift one foot off the ground and make circles with your ankle in one direction, and then in the other direction. Repeat on the other side.
It’s important to start slowly and gradually increase the intensity and duration of your exercises and stretches over time. It’s also important to wear proper footwear that supports your feet and provides adequate cushioning. If you are experiencing foot pain or other foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective exercises and stretches for your individual needs.
Foot massage

Foot massage can be a beneficial natural remedy for foot problems such as plantar fasciitis, heel pain, and general foot discomfort. Foot massage can help to promote relaxation, relieve pain, reduce muscle tension, and improve circulation in your feet. Use your hands or a massage ball to massage the soles of the feet and the arches.
Here are some foot massage techniques that can be helpful for foot problems:
- Arch massage: Sit in a chair and place a tennis ball or a small massage ball under the arch of your foot. Roll the ball back and forth under your foot, applying gentle pressure. This can help to stretch the plantar fascia and relieve tension.
- Toe stretches massage: Hold the heel of your foot with one hand and use the fingers of your other hand to stretch and massage each toe individually. This can help to improve flexibility and reduce tension in your toes.
- Heel massage: Use your thumbs to apply firm pressure to the bottom of your heel, moving in circular motions. This can help to reduce pain and inflammation in the heel.
- Ankle massage: Use your fingers to massage the area around your ankle, moving in circular motions. This can help to improve circulation and reduce stiffness in the ankle.
It’s important to communicate with your massage therapist about any foot problems you may be experiencing so they can tailor the massage to your individual needs. If you are massaging your own feet, start with light pressure and gradually increase the intensity as your feet become accustomed to the massage.
Foot massage can be a great way to relieve tension and promote relaxation in your feet, but it’s important to remember that it is not a substitute for medical treatment. If you are experiencing foot pain or other foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Proper footwear

Wearing properly fitting shoes with good arch support can help to prevent foot problems and alleviate pain. Choose shoes that are appropriate for the activity you plan to do. Proper footwear can play an important role in preventing and managing foot problems. Here are some tips on how to choose proper footwear to support healthy feet:
- Proper fit: Shoes that are too tight or too loose can cause a range of foot problems, including blisters, calluses, and ingrown toenails. Make sure to try on shoes later in the day when your feet are at their largest, and make sure there is a half inch of space between your longest toe and the end of the shoe.
- Arch support: Proper arch support can help prevent and manage conditions such as flat feet, plantar fasciitis, and overpronation. Look for shoes with a contoured footbed or insert that provides arch support.
- Cushioning: Shoes with good cushioning can help absorb shock and reduce impact when you walk or run. This can help prevent conditions such as heel pain and stress fractures. Look for shoes with thick soles or padded insoles.
- Breathability: Shoes that allow your feet to breathe can help prevent foot odor and fungal infections. Look for shoes made from breathable materials such as leather, mesh, or canvas.
- Roomy toe box: Shoes with a roomy toe box can help prevent conditions such as bunions and hammertoes. Look for shoes that allow your toes to move freely and do not squeeze or constrict them.
- Proper traction: Shoes with proper traction can help prevent slips and falls, especially on wet or slippery surfaces. Look for shoes with a non-slip sole or traction pads.
- Activity-specific: Choose shoes that are appropriate for the activity you will be doing. For example, running shoes should have different features than hiking boots or dress shoes.
Remember that the proper footwear is essential for maintaining healthy feet, but it is not a substitute for proper foot care and medical treatment. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Baking soda

Baking soda, also known as sodium bicarbonate, has many uses, including for foot care. Here are some ways baking soda can be used to help with foot problems:
- Foot soak: Adding baking soda to a foot soak can help soothe tired and achy feet, as well as reduce foot odor. Add 1/2 cup of baking soda to a basin of warm water and soak your feet for 15-20 minutes.
- Exfoliation: Baking soda can help exfoliate dry and rough skin on the feet. Mix 3 parts baking soda with 1 part water to make a paste, and then gently rub it onto your feet in circular motions. Rinse off with warm water and pat dry.
- Foot odor: Baking soda can help neutralize foot odor. Sprinkle baking soda into your shoes or directly onto your feet before putting on socks or shoes.
- Fungal infections: Baking soda has antifungal properties that can help treat fungal infections such as athlete’s foot. Mix 1 tablespoon of baking soda with 1 tablespoon of water to make a paste and then apply it to the affected area. Let it sit for 10-15 minutes before rinsing off with warm water.
While baking soda can be a useful home remedy for some foot problems, it is important to remember that it is not a substitute for proper medical treatment. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Corn starch

Corn starch is a fine, white powder made from corn and can be used in various ways to help with foot problems. Here are some ways corn starch can be used to benefit foot care:
- Foot odor: Corn starch can help absorb moisture and reduce foot odor. Sprinkle some corn starch on your feet or in your shoes to help absorb sweat and moisture.
- Blisters: Corn starch can help relieve pain and discomfort caused by blisters. Apply some corn starch onto the blistered area to help absorb moisture and reduce friction.
- Athlete’s foot: Corn starch can be used as a natural remedy for athlete’s foot. Mix some corn starch with water to make a paste and apply it to the affected area. Let it dry and then rinse off with warm water.
- Dry skin: Corn starch can help soothe and moisturize dry and cracked skin on the feet. Mix some corn starch with coconut oil or olive oil to make a paste and then apply it to your feet. Let it sit for a few minutes before rinsing off with warm water.
It is important to note that corn starch should not be used as a substitute for proper medical treatment for foot problems. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Vinegar

Vinegar has many uses, including for foot care. Here are some ways vinegar can be used to help with foot problems:
-
Athlete’s foot: Vinegar has antifungal properties that can help treat athlete’s foot. Mix equal parts of vinegar and water and soak your feet in the solution for 10-15 minutes, then rinse with water and dry thoroughly.
-
Foot odor: Vinegar can help reduce foot odor. Mix equal parts of vinegar and water and soak your feet in the solution for 15-20 minutes, then rinse with water and dry thoroughly.
-
Calluses and corns: Vinegar can help soften calluses and corns. Soak a cotton ball in vinegar and apply it to the affected area for 15-20 minutes, then use a pumice stone to gently exfoliate the dead skin.
-
Toenail fungus: Vinegar can also be used to treat toenail fungus. Soak your feet in a mixture of equal parts of vinegar and water for 15-20 minutes, twice a day. Dry your feet thoroughly after soaking.
It is important to note that vinegar should not be used as a substitute for proper medical treatment for foot problems. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Black tea

Black tea is known for its antioxidant and astringent properties, and it can be used in various ways to help with foot problems. Here are some ways black tea can be used for foot care:
-
Foot odor: Black tea can help reduce foot odor. Brew a few black tea bags in hot water for 10-15 minutes. Let the tea cool down and soak your feet in the solution for 20-30 minutes. Rinse with water and dry thoroughly.
-
Sweaty feet: Black tea can help reduce excessive sweating of the feet. Brew a few black tea bags in hot water for 10-15 minutes. Let the tea cool down and soak your feet in the solution for 20-30 minutes. Rinse with water and dry thoroughly.
-
Blisters: Black tea can help soothe and heal blisters. Soak a black tea bag in hot water for a few minutes, then let it cool down. Place the tea bag onto the blistered area and leave it on for 10-15 minutes.
-
Inflammation: Black tea can help reduce inflammation and swelling. Brew a few black tea bags in hot water for 10-15 minutes. Let the tea cool down and soak a towel in the solution. Wrap the towel around the affected area and leave it on for 15-20 minutes.
It is important to note that black tea should not be used as a substitute for proper medical treatment for foot problems. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Cypress

Cypress essential oil is known for its antibacterial, antifungal, and anti-inflammatory properties. It can be used in various ways to help with foot problems. Here are some ways cypress essential oil can be used for foot care:
- Foot odor: Cypress essential oil can help reduce foot odor. Add a few drops of cypress essential oil to a foot bath or mix it with a carrier oil like coconut oil and massage onto your feet.
- Sweaty feet: Cypress essential oil can help reduce excessive sweating of the feet. Add a few drops of cypress essential oil to a foot bath or mix it with a carrier oil and massage onto your feet.
- Fungal infections: Cypress essential oil can help fight fungal infections like athlete’s foot. Mix a few drops of cypress essential oil with a carrier oil and apply it to the affected area.
- Inflammation: Cypress essential oil can help reduce inflammation and swelling. Mix a few drops of cypress essential oil with a carrier oil and massage onto the affected area.
It is important to note that cypress essential oil should not be used as a substitute for proper medical treatment for foot problems. If you are experiencing foot problems, it is important to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs.
Insoles

Insoles are a common solution for foot problems. They are designed to provide additional support, cushioning, and shock absorption to the feet. Here are some ways insoles can be helpful for foot problems:
- Arch support: Insoles can provide additional support to the arch of the foot, which can be helpful for individuals with flat feet or fallen arches.
- Plantar fasciitis: Insoles can be designed to provide additional cushioning and support to the heel and arch, which can be helpful for individuals with plantar fasciitis.
- Metatarsalgia: Insoles can help redistribute pressure across the foot, which can be helpful for individuals with metatarsalgia (pain in the ball of the foot).
- Foot fatigue: Insoles can provide additional shock absorption and cushioning, which can help reduce foot fatigue and improve overall comfort.
It is important to choose the right type of insole for your individual needs. There are a variety of insoles available on the market, ranging from basic foam insoles to custom-made orthotics. It is recommended to consult with a healthcare provider or a podiatrist to determine the best type of insole for your specific foot problem.
How to buy proper fitting shoes

Buying properly fitting shoes is important for foot health and comfort. Here are some tips to help you find the right fit:
- Measure your feet: Get your feet measured by a professional or use a foot measuring device to determine your correct shoe size. Your shoe size can change over time, so it’s important to get measured periodically. Measure both feet every time you buy new shoes
- Try on shoes at the end of the day: Your feet may swell throughout the day, so it’s best to try on shoes in the late afternoon or evening when your feet are at their largest.
- Wear the socks you plan to wear with the shoes: Wear the same type of socks you plan to wear with the shoes to ensure a proper fit.
- Stand up when trying on shoes: Stand up and walk around in the shoes to see how they feel. Make sure there is enough room in the toe box and that the shoes feel comfortable and supportive.
- Check for proper fit: Make sure there is a half inch of space between your longest toe and the end of the shoe. The shoes should fit snugly around the heel and midfoot but not be too tight or too loose. The joint where the foot attaches to your ties should be the widest part of the shoe without being squeezed. Look for shoes with wide toe room
- Test the shoes on different surfaces: Walk around on different surfaces to ensure that the shoes provide enough support and stability. Try on both shoes and walk on a hard surface
- Consider the type of activity: Choose shoes that are appropriate for the activity you plan to do. Running shoes, for example, may be designed differently than hiking shoes.
It’s also important to replace your shoes regularly, as shoes can lose their support and cushioning over time. If you have any foot problems or concerns, it’s best to consult with a healthcare provider or a podiatrist for guidance on choosing the right shoes for your needs.
Myth: Magnets and foot problems

There is a common myth that magnets can be used to treat foot problems such as plantar fasciitis, heel pain, and flat feet. However, there is little scientific evidence to support these claims. While some people may report feeling relief from foot pain after using magnetic insoles or other magnetic devices, the evidence is anecdotal, and the effects may be due to a placebo effect or other factors.
It’s important to note that foot problems can have a variety of causes, and the most effective treatments will depend on the underlying condition. In some cases, lifestyle changes, physical therapy, or other interventions may be more effective than magnetic therapy. If you are experiencing foot pain or other foot problems, it’s best to consult with a healthcare provider or a podiatrist for guidance on the most effective treatments for your individual needs. They can help you determine the underlying cause of your foot problem and recommend the most appropriate course of treatment.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

