Corns Treatment Guide: From Home Remedies to Professional Care
Corns and calluses are thickened areas of skin that develop in response to pressure or friction. They are commonly found on the hands and feet, particularly on the palms, fingers, soles, and toes. While they may be similar in appearance and treatment, they are different in their location and causes. We will discuss the following topics:
Overview of Corns
Overview of Calluses
Symptoms of calluses
Causes of calluses
How to prevent corns and calluses
How corns and calluses are managed
When to seek urgent medical care
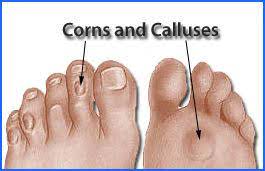
Corn
Calluses
Calluses are broader patches of thickened skin that commonly develop on the soles of the feet or the palms of the hands. Unlike corns, they’re generally not painful, though they can be uncomfortable or visually unappealing. These areas of thickened skin result from repetitive friction or pressure, often experienced during activities like walking or using hand tools without adequate protection. Calluses typically present as large, hard, and rough lumps with a yellowish or grayish hue, and they’re primarily managed by addressing the underlying causes of friction or pressure.
The symptoms of corns and calluses may include:
- Pain or discomfort: Corns and sometimes calluses can cause pain or discomfort, especially when pressure is applied.
- Thickened skin: Both corns and calluses are characterized by areas of thickened skin, which may feel hardened to the touch.
- Raised bumps: Corns often present as raised bumps on the skin, while calluses typically form broader, flatter patches.
- Coloration: Corns can vary in color, with hard corns often appearing yellowish or grayish, while calluses may have a similar coloration.
- Location: Corns are more likely to develop on the tops or sides of toes, while calluses commonly form on the soles of the feet or the palms of the hands.
- Discomfort while walking: Both corns and calluses may cause discomfort or pain, particularly when walking or wearing tight footwear.
The causes of corns and calluses include:
- Friction or pressure: The primary cause of both corns and calluses is repetitive friction or pressure on the skin. This often occurs from wearing ill-fitting shoes, walking barefoot, or engaging in activities that involve repetitive movements or pressure on specific areas of the hands or feet.
- Foot deformities: Certain foot deformities, such as hammer toes or bunions, can increase the likelihood of developing corns or calluses. These deformities can cause bones to press against the skin, leading to increased friction and pressure.
- Improper footwear: Wearing shoes that are too tight, too loose, or have high heels can contribute to the development of corns and calluses. Tight shoes can compress the toes, while loose shoes can cause rubbing and friction.
- Occupational factors: People who work in professions that involve standing for long periods or using hand tools without proper protection are at increased risk of developing calluses on their feet or hands.
- Sports or activities: Participation in certain sports or activities, such as running, dancing, or playing musical instruments, can increase the likelihood of developing corns or calluses due to repetitive movements or pressure on specific areas of the hands or feet.
- Age: As people age, the skin tends to become drier and less elastic, making it more susceptible to developing corns and calluses.
- Reduced sensation: Conditions that reduce sensation in the feet, such as diabetes or peripheral neuropathy, can increase the risk of developing corns and calluses because the affected individuals may not feel discomfort until the condition has progressed.
How to prevent corns and calluses
Preventing corns and calluses involves taking proactive measures to reduce friction and pressure on the skin. Here are some tips:
- Wear properly fitting shoes: Choose shoes that provide adequate room for your toes and avoid tight or narrow footwear. Ensure there is enough space between your toes and the shoe’s material to prevent rubbing.
- Use protective padding: Cushioning pads or insoles can help distribute pressure and reduce friction on vulnerable areas of the feet. Apply them to areas prone to corns or calluses, such as the toes or balls of the feet.
- Keep feet dry and moisturized: Moisturize your feet regularly to prevent dry, cracked skin, which can increase the risk of corns and calluses. However, ensure your feet are dry before wearing socks or shoes to avoid moisture-related issues.
- Avoid going barefoot: Walking barefoot increases the likelihood of friction and pressure on the soles of the feet, leading to the development of calluses. Wear socks or supportive footwear, especially in high-traffic areas.
- Trim toenails properly: Trim your toenails straight across to prevent them from digging into adjacent toes and causing corns. Avoid cutting them too short or rounding the edges, as this can lead to ingrown toenails.
- Choose appropriate socks: Opt for socks made of breathable materials that wick moisture away from the skin. Avoid wearing socks with seams that may rub against your toes.
- Address foot deformities: If you have foot deformities such as bunions or hammer toes, consult a healthcare professional for appropriate treatment options. Addressing these issues can reduce the risk of developing corns and calluses.
- Inspect your feet regularly: Check your feet regularly for any signs of redness, irritation, or skin thickening. Early detection allows for prompt intervention and prevents the worsening of corns and calluses.
How corns and calluses are managed

Managing corns and calluses involves addressing the underlying causes of friction and pressure while also providing relief from discomfort. Here are some strategies for managing these skin conditions:
- Wear proper footwear: Invest in shoes that fit well and provide ample space for your toes. Avoid high heels and shoes with narrow toe boxes, as they can exacerbate corns and calluses.
- Use protective padding: Apply cushioning pads or moleskin to areas prone to corns and calluses to reduce friction and pressure. These pads can provide immediate relief and prevent further irritation.
- Soak and exfoliate: Soak your feet in warm, soapy water to soften the skin, then gently exfoliate with a pumice stone or foot file to remove dead skin buildup. This can help smooth rough patches and reduce the size of corns and calluses.
- Apply moisturizer: Keep the skin hydrated by applying moisturizer regularly. This helps prevent dryness and cracking, which can contribute to the formation of corns and calluses.
- Trim excess skin: If corns or calluses become too thick or painful, consult a healthcare professional. They can safely trim the excess skin using sterile instruments to relieve discomfort.
- Medicated treatments: Over-the-counter treatments such as corn pads, callus removers, or salicylic acid plasters can help soften corns and calluses. Follow the instructions carefully and avoid using these products on open or infected skin.
- Orthotic devices: Custom orthotic inserts or shoe modifications can redistribute pressure on the feet and alleviate discomfort associated with corns and calluses. A podiatrist or orthopedic specialist can recommend appropriate devices based on your individual needs. If prescribed orthotic inserts or shoe modifications, wear them consistently to redistribute pressure on the feet and prevent recurrence of corns and calluses.
- Address foot deformities: If corns or calluses are caused by underlying foot deformities such as bunions or hammer toes, seek treatment to correct these issues. This may involve wearing splints or undergoing surgery to realign the affected joints.
Taking appropriate precautions is crucial for managing corns and calluses effectively and preventing complications. Here are some important precautions to consider:
- Avoid self-treatment: Refrain from attempting to cut or shave corns or calluses on your own, as this can lead to infection or further skin damage. Seek guidance from a healthcare professional for safe and appropriate treatment.
- Regular foot inspections: Check your feet regularly for signs of redness, irritation, or skin thickening. Early detection allows for prompt intervention and prevents the worsening of corns and calluses.
- Keep the skin hydrated by applying moisturizer regularly, especially after soaking or exfoliating. However, avoid moisturizing between the toes, as excessive moisture can increase the risk of fungal infections.
- Replace protective padding as needed and avoid using adhesive products on open or irritated skin.
- Address underlying conditions: Seek treatment for any underlying foot deformities or medical conditions that contribute to the development of corns and calluses, such as bunions, hammer toes, diabetes, or peripheral neuropathy.
- Practice good foot hygiene: Keep your feet clean and dry and avoid walking barefoot in public places to reduce the risk of infection. Dry your feet thoroughly, especially between the toes, after bathing or swimming.
- Seek professional advice: Consult a healthcare professional if you experience severe pain, discomfort, or signs of infection associated with corns and calluses. They can provide personalized recommendations and interventions to address your specific needs.
Seek urgent medical care for corns and calluses if you experience any of the following:
- Diabetic: If you have diabetes, it’s crucial to seek prompt medical attention for any foot issues, including corns and calluses. Diabetes can impair circulation and sensation in the feet, increasing the risk of complications such as infection or ulceration.
- Poor circulation: Individuals with poor circulation, such as those with peripheral arterial disease, should seek medical attention if they develop corns or calluses. Poor circulation can delay healing and increase the risk of complications.
- Presence of bloody or pus-like discharge: If a corn or callus becomes infected, it may produce discharge that is bloody or pus-like. Seek medical attention immediately for proper evaluation and treatment of the infection.
- Lasts more than 3 weeks: If a corn or callus persists for more than three weeks despite home treatment, it’s essential to consult a healthcare professional. Persistent corns or calluses may require medical intervention to address underlying issues.
- Accompanied by severe pain: Severe pain associated with a corn or callus may indicate an underlying problem, such as infection or nerve involvement. Seek medical attention for evaluation and management of the pain.
- The corn or callus recurs: If a corn or callus keeps coming back despite treatment, it may indicate an unresolved issue that requires medical attention. A healthcare professional can help identify and address the underlying cause of recurrence.
- Discomfort in a diabetic or immunocompromised individual: Individuals with diabetes or compromised immune systems should seek medical care for even minor foot issues to prevent complications.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

