Types of Contraceptives: Pills, IUDs, Condoms, and More
Contraceptives are an important part of reproductive health care. They provide a safe and effective way to prevent unwanted pregnancy and can also help to protect against sexually transmitted infections. Contraceptives come in many forms, including birth control pills, intrauterine devices, condoms, diaphragms, and spermicide. Each of these methods has its own advantages and disadvantages, so it is important to discuss the right contraceptive option with a healthcare provider. With the right choice, contraceptives can help people make informed decisions about their reproductive health. Please keep reading for details on the following topics:
Rhythm method
Standard days method
Hormonal methods
Lactational amenorrhea method
Barrier methods
Birth control pills
Birth control injections
Vaginal rings
Sterilization
Emergency contraception
Choosing a contraception method
Calendar (rhythm) method
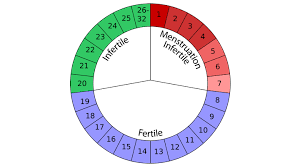
The Calendar (or Rhythm) Method is a natural family planning approach that helps couples to predict when a woman is most likely to become pregnant. It is based on tracking the length of a woman’s menstrual cycle, and the days when she is most likely to become pregnant. This method is popular among couples who prefer a natural approach to family planning, and it can be used to prevent or achieve pregnancy. To use the Calendar Method, couples track the length of the woman’s menstrual cycle and record the first day of her period. They also note the length of the cycle, which can vary from month to month. By tracking the cycle, couples can calculate the days when the woman is most likely to become pregnant. The Calendar Method is a safe and effective way to plan a pregnancy or prevent one.
The calendar (rhythm) method technique
This method helps individuals identify the window of fertility within their menstrual cycle, aiding in family planning or contraception strategies. This explanation outlines a method for determining the fertile period within a woman’s menstrual cycle:
- Recording Menstrual Periods: Over a span of 6 to 8 months, each menstrual period’s start and end dates are documented.
- Assessing Cycle Regularity and Length: By observing the patterns over this period, one can determine if the menstrual cycle is regular and the typical duration of the cycle.
- Calculating Fertile Period:
- First Day of Fertile Period: Subtracting 18 days from the number of days in the shortest menstrual cycle provides the starting point for the fertile period. This represents the number of days after the menstrual period ends.
- Last Day of Fertile Period: Subtracting 11 days from the number of days in the longest menstrual cycle gives the end point for the fertile period. This value corresponds to the number of days after the menstrual period begins.
- Correlation with Menstrual Period: The obtained numbers align with days relative to the start and end of the menstrual period, respectively.
Standard days method (SDM)

The Standard Days Method (SDM) is a contraceptive technique that helps couples plan or prevent pregnancy. It relies on regular menstrual cycles and is based on the couple’s mutual agreement to abstain from unprotected sex on certain days of the month. The Standard Days Method is a simple, safe and natural way to plan a family and is 99% effective when used correctly. It can be used by all couples, regardless of age or religion, and is especially helpful for those who cannot or do not want to use other forms of contraception. It makes use of cycle beads as a contraceptive method and it involves tracking the menstrual cycle using a string of beads, each representing one day.
- Each bead corresponds to one day of the menstrual cycle, helping track fertile and non-fertile days.
- Unprotected sex is permitted during days 1 to 7 of the menstrual cycle, which typically represents the least fertile period.
- Intercourse should be avoided on days 8 to 19, considered the fertile window when pregnancy is more likely.
- The cycle concludes on day 20, suggesting the return to a lower risk period, allowing for unprotected sex if desired.
HORMONAL METHODS

Hormonal methods of contraception are a popular and effective way to prevent pregnancy. These methods work by using hormones such as estrogen and progestin to stop ovulation, thicken cervical mucus and thin the uterine lining, making it difficult for sperm to reach or fertilize an egg. Hormonal methods can be taken in the form of pills, patches, implants, shots, and vaginal rings, giving individuals the flexibility to choose the method that works best for them. With correct and consistent use, hormonal methods are over 99% effective in preventing pregnancy.
Implants:
-
- Implants release progestin, a hormone, to prevent pregnancy.
- They offer protection for up to three years.
Intrauterine Contraceptive Device (IUCD):
-
-
- A small device inserted into the womb.
- Provides contraceptive protection for about 3 to 10 years.
-
Estrogen only pills
The Estrogen Only Pill is a type of birth control pill that contains only estrogen, as opposed to combination birth control pills, which contain both estrogen and progestin. Estrogen only pills are typically prescribed to women who have reached menopause or have had a hysterectomy, as they no longer need progestin to regulate their hormones. While estrogen only pills are an effective form of birth control and can help regulate hormones and reduce symptoms of menopause, it is important to consult with your doctor to determine whether this form of contraception is right for you.
Progestin-only pills contain progesterone
Progestin-only pills (also known as the “mini-pill”) are effective contraceptives that provide women with a low-dose, hormone-only form of birth control. Unlike combination oral contraceptives, which contain both progestin and estrogen, progestin-only pills contain just one hormone, progestin, which helps to prevent pregnancy by thickening a woman’s cervical mucus and stopping the release of eggs from the ovaries. They are easy to use, have a high success rate, and are considered safe for most women. Progestin-only pills are a great option for women who cannot use combination birth control pills due to health reasons, or for those who do not want to take estrogen.
Combination pills are taken at the same time daily.
Combination pills are a popular choice for those looking to take multiple medications in a single dose. Combination pills consist of two or more active ingredients in a single tablet, capsule, or liquid form. This type of medication is typically used to treat complex health conditions, as it can provide a more effective and convenient way to manage multiple medications. Combination pills can also reduce the risk of medication errors, as the patient only needs to take one pill instead of multiple individual medications.
Combination of estrogen and progestin-only
Combination of estrogen and progestin-only is a combination of two hormones that can be used to treat a variety of health concerns. This combination of hormones has been found to have a positive effect on the body, and can help to reduce the risk of certain health conditions such as heart disease, stroke, breast cancer, and osteoporosis. The hormones in this combination work together to provide a balanced, safe, and effective treatment for many conditions, and can help to improve overall health and well-being.
Patches
Patches are hormonal contraceptives that deliver hormones through the skin. These small, adhesive patches are typically applied to the skin once a week for three weeks, followed by a patch-free week to allow for menstruation. They release estrogen and progestin into the bloodstream, inhibiting ovulation and thickening cervical mucus to prevent sperm from reaching the egg. Patches are convenient and effective when used correctly, offering an alternative to daily oral contraceptives. However, they may cause skin irritation at the application site, and users must remember to change the patch weekly to maintain effectiveness.
Vaginal rings
Vaginal rings are contraceptives designed to provide long-term protection against unplanned pregnancy. They are hormone-releasing contraception devices that are placed inside the vagina and remain in place for three weeks. Vaginal rings slowly release a low number of hormones that prevent ovulation, thereby reducing the risk of pregnancy. While vaginal rings can be an effective form of contraception, it is important to note that they do not protect against sexually transmitted infections. These rings must be changed every month.
Birth control pills
Birth control pills are a commonly used form of contraception. They are small tablets taken orally and they contain hormones that prevent pregnancy. Birth control pills work by preventing ovulation, thickening cervical mucus to block sperm, and thinning the lining of the uterus to reduce the chance of implantation. This makes it much less likely that a pregnancy will occur. Birth control pills are highly effective when taken correctly and can provide women with long-term protection from pregnancy. These pills must be taken at the same time every day.
Birth control injections
Birth control injections are a convenient and effective form of contraception. These injections, also known as Depo-Provera, contain a hormone called progestin which helps to prevent pregnancy by suppressing ovulation and thickening cervical mucus to block sperm. The injection is administered into the arm or buttocks every three months and is 99% effective in preventing pregnancy. Birth control injections provide a reliable form of contraception, with the added bonus of no daily pill reminders.
BARRIER METHODS
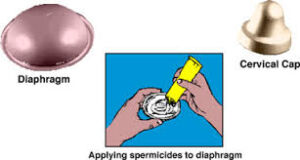
Barrier methods are a form of contraception that provide a physical barrier between sperm and egg, preventing pregnancy. Barrier methods include condoms, diaphragms, sponges, cervical caps, and spermicides. Condoms are the most popular and widely used form of barrier contraception, as they not only protect against unwanted pregnancy, but also provide protection against the transmission of sexually transmitted infections. Diaphragms and cervical caps are silicone cups that are inserted into the vagina and must be used with spermicide for effectiveness. Sponges are small, soft sponges that are inserted into the vagina and must also be used with spermicide. Spermicide is a chemical that kills sperm. Barrier methods are an effective form of contraception when used correctly and consistently.
Condoms
Condoms are one of the most popular and effective forms of birth control and sexually transmitted infection (STI) prevention. They are thin, stretchy pouches made from latex, plastic, or lambskin that are designed to fit over the penis during intercourse. Condoms create a physical barrier that helps prevent sperm from entering the uterus and fertilizing an egg. They also help protect against the transmission of STIs, including HIV. When used correctly, condoms are an extremely effective form of contraception and STI prevention. Condoms are designed for the male or female and reduces the risk of transmitting infection during intercourse.
Lactational amenorrhea method (LAM)
Lactational amenorrhea method (LAM) is an evidence-based, natural method of contraception that uses the temporary infertility that occurs during breastfeeding. It is a safe and effective way to delay or avoid pregnancy and can be used for the first six months after childbirth. This method relies on three criteria that must be met in order to be effective: exclusive breastfeeding, amenorrhea, and timing of breastfeeding. With LAM, breastfeeding must be exclusive and frequent, meaning that only breastmilk is being given and that the baby is breastfeeding at least every four to six hours during the day and at least every six hours at night. In addition, amenorrhea must be present, meaning that you must not have had your menstrual period return. Lastly, timing of breastfeeding is important, as the baby must be less than six months old, and breastfeeding must occur at least every four to six hours during the day and at least every six hours at night. If all three criteria are met, LAM is an effective method of contraception with a failure rate of less than two percent.
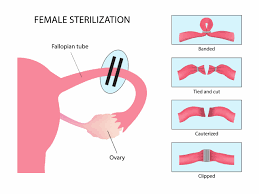
STERILIZATION
Sterilization is a permanent method typically considered when individuals or couples who have decided on having no more children. It is intended to prevent pregnancy by permanently blocking the fallopian tubes in women or the vas deferens in men. In women, sterilization is often performed through a procedure called tubal ligation, where the fallopian tubes are either cut, tied, or sealed to prevent eggs from reaching the uterus. In men, sterilization, known as a vasectomy, involves cutting or blocking the vas deferens to prevent sperm from being ejaculated. Sterilization procedures are highly effective and considered permanent, although they can sometimes be reversed through surgical procedures. It’s essential to carefully consider sterilization as it is meant to be irreversible.
Vasectomy is a permanent form of birth control for men that involves the surgical interruption of the vas deferens, the tubes that carry sperm from the testicles to the penis. Vasectomy works by blocking the tube carrying the male semen. The procedure is quick and relatively painless, and results in a man producing no sperm and being permanently sterile. Vasectomy is an effective form of contraception that has been used for many decades and is considered to be one of the safest and most cost-effective forms of birth control. The procedure itself is typically done in an outpatient setting, and recovery time is usually minimal.
Hysterectomy or removal of the womb
Hysterectomy, the surgical removal of the uterus, is a common gynecological procedure. It is typically performed to treat a variety of conditions, including uterine fibroids, endometriosis, uterine prolapse, and cancer. While hysterectomy has been known to provide relief from symptoms, it is a major surgery and should be discussed with your healthcare provider to determine if it is the right option for you. There are several types of hysterectomy, including total, subtotal, radical, and laparoscopic, each with their own risks and benefits. Recovery time varies depending on the type of procedure performed and can take up to six weeks or more.
Tuba ligation (TL) or tying the fallopian tubes
Tubal ligation, also known as “tying the tubes,” is a permanent form of birth control. It is a surgical procedure in which a woman’s fallopian tubes are blocked, tied, or sealed to prevent eggs from traveling from the ovaries to the uterus. This procedure can be done using clips, rings, or by cutting and sealing the fallopian tubes with an electric current. The procedure is safe and typically has few complications, making it a popular choice for women who wish to permanently prevent pregnancy.
FACTORS INHIBITING THE CHOICE OF CONTRACEPTION
These factors require careful consideration when selecting a contraceptive method to ensure safety and effectiveness. Consulting with a healthcare provider is crucial for personalized recommendations.
Smoking increases the risk of cardiovascular issues, particularly when using hormonal contraceptives.
Migraines, especially those with aura, may pose an increased risk of stroke when combined with hormonal contraception.
Diabetes can affect the body’s response to hormonal birth control.
After childbirth, hormonal changes and breastfeeding can impact contraceptive choices, requiring careful consideration for the mother’s health and breastfeeding goals.
Age: Certain contraceptive methods may not be suitable for younger adolescents or older individuals due to safety concerns or effectiveness.
Medical Conditions: Certain medical conditions or medications may interact with contraceptive methods, affecting their efficacy or safety.
Allergies or Sensitivities: Allergies or sensitivities to contraceptive ingredients may limit the choice of methods available.
Cultural or Religious Beliefs: Cultural or religious beliefs may influence an individual’s acceptance or rejection of certain contraceptive methods.
WHEN CHOOSING A CONTRACEPTIVE METHOD, ONE SHOULD CONSIDER

Choosing a contraceptive method can be a difficult decision. With so many options available, it can be hard to know which one is best for you. Whether you’re considering a hormonal method, an intrauterine device (IUD), or a barrier method, it’s important to take the time to evaluate your needs and research the various options available. When choosing a contraceptive method, several factors should be considered:
-
Medical benefits: Evaluate how the contraceptive method may positively impact your health, such as regulating menstrual cycles or reducing the risk of certain conditions like ovarian cysts or endometriosis.
- Price: Consider the cost of the contraceptive method, including any associated healthcare visits or prescriptions, and ensure it fits within your budget.
- Future plans to get pregnant: Determine whether you plan to conceive in the near future, as some contraceptive methods may have temporary effects on fertility, while others may be easily reversible.
- Side effects: Understand the potential side effects associated with each contraceptive method, such as changes in menstrual bleeding, mood swings, or weight gain, and consider how they may affect your daily life.
-
Advantages and disadvantages: Evaluate the pros and cons of each contraceptive method based on factors like effectiveness, ease of use, frequency of administration, and any personal preferences or lifestyle considerations.
EMERGENCY CONTRACEPTION

Emergency contraception is an effective option for preventing unintended pregnancies. It can be used up to five days after unprotected intercourse or a contraceptive failure and can be used both before and after ovulation. Emergency contraception can be taken as a pill or inserted as an intrauterine device (IUD). It works by delaying or preventing ovulation and preventing fertilization. However, it cannot disrupt an already-established pregnancy. It is important to note that emergency contraception is not the same as the abortion pill, and it should not be used as a regular form of birth control. Emergency contraception is a great option for those in need of short-term protection from an unintended pregnancy.
Times when an emergency contraception can be used
In situations where contraceptives methods fail or are not used correctly, emergency contraception may be considered. Here are some scenarios and corresponding options:
- If a condom breaks and one forgot to take the birth control pill:
- Emergency contraception pills (ECPs), commonly known as the “morning-after pill,” can be taken within 72 hours (or up to 120 hours or 5 days depending on the type) after unprotected intercourse to help prevent pregnancy.
- Had sex without using protection:
- In this case, if there’s a concern about the risk of pregnancy, emergency contraception pills should be considered as soon as possible.
- Taking medication that interferes with contraceptives pills:
- Some medications, such as certain antibiotics, anticonvulsants, or antiretrovirals, may reduce the effectiveness of hormonal contraceptives like birth control pills. If taking such medications, additional contraceptive measures like condoms or alternative forms of contraception may be recommended. Additionally, consulting a healthcare provider for personalized advice is crucial.
It’s important to note that emergency contraception is not 100% effective and should not be relied upon as a regular form of birth control. Consistent and correct use of contraceptives, along with open communication with healthcare providers, is key to preventing unintended pregnancies. If there are concerns about contraceptives failure or unplanned pregnancy, seeking advice from a healthcare professional is recommended.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions. contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives contraceptives


