Cervical Cancer Awareness: Understanding Prevention and Early Detection
Cervical cancer is a type of cancer that develops in a woman’s cervix, the lower part of the uterus that connects to the vagina. This type of cancer is usually caused by the human papillomavirus (HPV) and the uncontrollable growth of cells in the cervix. Cervical cancer can be detected early and treated, but if left unchecked it can spread to other parts of the body and become more difficult to treat. Treatment options for cervical cancer include chemotherapy, radiation, and surgery. Early detection of cervical cancer is critical in order to reduce the risk of developing a more aggressive form of the disease. Please keep reading for details on the following topics:
Overview of the cervix
Signs and symptoms of cervical cancer
Causes of cervical cancer
Risk factors for cervical cancer
Stages of cervical cancer
Diagnosis of cervical cancer
Prevention of cervical cancer
Treatment of cervical cancer
Guidelines for cancer screening
When to seek urgent medical care

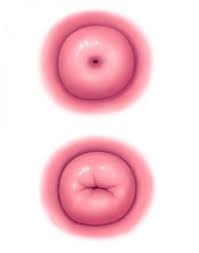
Overview of the cervix
The cervix, part of the female reproductive system, is a cylindrical shaped organ located at the bottom of the uterus. It opens up into the vagina and serves an important role in both fertility and childbirth. During childbirth, the cervix dilates to allow the baby to move through the birth canal. During fertility, the cervix produces mucus that helps to transport sperm to the uterus. In addition, the cervix is also an important part of the menstrual cycle, as it helps regulate and control the amount of menstrual fluid. Let’ describe the cervix further:
-
It is a part of the uterus (the area which houses the growing baby during pregnancy):
- The uterus, also known as the womb, is an organ in the female reproductive system where the fertilized egg implants and grows into a fetus during pregnancy. It is divided into several parts, including the fundus (upper part), body (central part), and cervix (lower part). During pregnancy, the uterus expands to accommodate the growing fetus, providing a nurturing environment for its development.
- The cervix is located in the lowest segment of the uterus:
- The cervix is the lower portion of the uterus that protrudes into the vagina. It serves as a gateway between the uterus and the vagina. The cervix contains a small opening called the cervical canal, which allows menstrual blood to flow out of the uterus during menstruation and provides a passage for sperm to enter the uterus during intercourse. During pregnancy, the cervix remains closed to help support and protect the developing fetus within the uterus.
-
The cervix is the opening of the uterus which allows the baby to pass through:
- This refers to the cervix’s role during childbirth. As labor progresses, the cervix undergoes a process called dilation and effacement, where it gradually opens (dilates) and thins out (effaces) to allow the baby to pass through the birth canal (vagina) and be born. This opening of the cervix during childbirth is crucial for the safe delivery of the baby.
Signs and symptoms of cervical cancer
It is important to know when to seek urgent medical care, as delaying appropriate treatment can lead to further health complications. If you experience any of the following symptoms, you should seek medical help immediately. If you have any doubts about whether you should seek medical care, it is always better to err on the side of caution and consult with your doctor.
- Heavy, watery, or bloody vaginal discharge:
- This may indicate abnormal changes in the cervix or uterus. In cervical cancer, such discharge can result from the presence of cancerous cells in the cervix.
- Offensive discharge:
- Foul-smelling discharge can be a sign of infection or cervical cancer. It’s essential to seek medical attention if this symptom persists.
- Vaginal bleeding after intercourse, between menstrual periods, or after menopause:
- Bleeding outside of normal menstruation or after menopause can be concerning. It may indicate cervical cancer, especially if it occurs after menopause.
- Heavy menstrual periods:
- While heavy periods can be common for some women, unusually heavy bleeding may suggest an underlying issue such as cervical cancer or uterine fibroids.
Causes of cervical cancer
The Human Papilloma Virus (HPV): Human Papillomavirus (HPV) is the primary cause of cervical cancer. HPV is a common sexually transmitted infection that can infect cells on the surface of the skin and those lining the genitals, including the cervix. Persistent infection with high-risk strains of HPV, particularly HPV types 16 and 18, can lead to changes in cervical cells, potentially progressing to cervical cancer over time. It’s important to note that not all HPV infections lead to cancer, and many clear up on their own without causing any harm. However, regular screening and vaccination against HPV can significantly reduce the risk of cervical cancer.
Risk factors for cervical cancer
These are recognized risk factors for developing cervical cancer:
- HPV infection: Human Papillomavirus (HPV) infection, especially with high-risk strains, is the most significant risk factor for cervical cancer.
- Multiple sexual partners: Engaging in sexual activity with multiple partners increases the likelihood of HPV exposure, thus elevating the risk of cervical cancer.
- Smoking: Tobacco use, including smoking, is associated with an increased risk of cervical cancer. Chemicals in tobacco can damage cervical cells and weaken the immune system’s ability to fight HPV infection.
- HIV infection: Human Immunodeficiency Virus (HIV) weakens the immune system, making individuals more susceptible to HPV infection and less capable of fighting HPV-related abnormalities, which can progress to cervical cancer.
- Use of birth control pills: Long-term use of oral contraceptives (birth control pills) has been linked to a slightly increased risk of cervical cancer. However, this risk typically diminishes after discontinuation of the pill.
- Having multiple children: Some studies suggest that giving birth to multiple children may slightly increase the risk of developing cervical cancer. The exact mechanism behind this association is not fully understood.
-
Family history of cervical cancer: A family history of cervical cancer or certain genetic factors may contribute to an increased risk of developing the disease. However, most cases of cervical cancer occur in individuals without a family history of the condition.
Stages of cervical cancer
These descriptions outline the stages of cervical cancer:
- Stage I: At this stage, cancer is localized and confined to the cervix. It has not spread to nearby tissues or organs. Treatment options often involve surgery or radiation therapy to remove or destroy the cancerous cells.
- Stage II: Cancer has progressed beyond the cervix and uterus but has not spread to the pelvic wall or other distant organs. Treatment typically involves a combination of surgery, radiation therapy, and possibly chemotherapy to target the cancerous cells and prevent further spread.
- Stage III: Cancer has spread to the lower part of the vagina, pelvic wall, ureters (tubes that carry urine), and nearby lymph nodes. Treatment may include a combination of surgery, radiation therapy, and chemotherapy to shrink tumors, relieve symptoms, and prevent further spread of the disease.
-
Stage IV: Cancer has advanced to the bladder, rectum, or other parts of the body beyond the pelvis. Treatment options may focus on palliative care to manage symptoms and improve quality of life. This stage may involve a combination of surgery, radiation therapy, chemotherapy, and other targeted therapies to slow the progression of the disease and alleviate discomfort.

These are diagnostic procedures and tests commonly used in the evaluation of cervical cancer:
-
Biopsy (the collection of a sample of tissue): A biopsy involves the removal of a small sample of tissue from the cervix or other potentially affected areas for examination under a microscope. This helps in confirming the presence of cancer cells and determining the cancer type and grade.
- Pap smear: Also known as a Pap test, this screening procedure involves collecting cells from the cervix and examining them under a microscope to detect any abnormal changes. Pap smears can identify precancerous or cancerous cells in the cervix, allowing for early detection and intervention.
- Liver and kidney function studies: These tests evaluate the function of the liver and kidneys by measuring levels of specific enzymes, proteins, and waste products in the blood. Abnormal results may indicate the presence of metastases or complications related to cervical cancer.
- Blood and urine tests: Blood tests may be performed to assess various parameters, such as complete blood count (CBC), tumor markers, and human chorionic gonadotropin (hCG) levels. Urine tests may also be conducted to detect abnormal substances that could indicate kidney or bladder involvement.
- X-rays of your bladder, rectum, bowels, and abdominal cavity: X-rays may be used to visualize the internal structures of the bladder, rectum, bowels, and abdominal cavity to identify any abnormalities or signs of metastasis.
- Scans (CT scan, MRI scan, PET scan, chest X-ray): Imaging studies such as CT (computed tomography), MRI (magnetic resonance imaging), and PET (positron emission tomography) scans provide detailed images of the internal organs and tissues, helping to determine the extent of cancer spread (staging) and guide treatment decisions. Chest X-rays may also be performed to evaluate the lungs for metastases.
-
An internal examination of the vagina and cervix: A pelvic examination, including a visual inspection and manual palpation of the vagina and cervix, allows healthcare providers to assess the size, shape, and texture of any abnormalities, such as tumors or lesions.
How to prevent cervical cancer
These are preventive measures to reduce the risk of cervical cancer:
-
Receiving regular Pap tests or Pap smear: Regular screening with Pap tests or Pap smears can detect abnormal cervical cells early, allowing for timely intervention and reducing the risk of cervical cancer development.
- Practicing safe sex: Practicing safe sex, including the consistent and correct use of condoms, reduces the risk of HPV infection, which is the primary cause of cervical cancer.
- Being vaccinated against HPV: HPV vaccination provides protection against several high-risk strains of the virus, significantly reducing the risk of cervical cancer and other HPV-related diseases. Vaccination is typically recommended for adolescents and young adults before they become sexually active.
- Using condoms or other barrier methods: Using condoms or other barrier methods during sexual activity can reduce the risk of HPV transmission and other sexually transmitted infections, thereby lowering the risk of cervical cancer.
- Limiting sexual partners: Limiting the number of sexual partners and engaging in mutually monogamous relationships can reduce the risk of HPV exposure and transmission, thereby decreasing the risk of cervical cancer.
-
Avoiding smoking and using tobacco products: Smoking is associated with an increased risk of cervical cancer, as it can weaken the immune system and promote the progression of HPV-related cervical abnormalities. Avoiding smoking and tobacco products can help reduce the risk of developing cervical cancer.
Treatment of cervical cancer depends on:
These factors influence the treatment decisions for cervical cancer:
- The size and type of cervical cancer a person has: The size and type of cervical cancer, such as squamous cell carcinoma or adenocarcinoma, influence the choice of treatment. For example, smaller tumors may be treated with surgery or radiation therapy, while larger tumors may require a combination of treatments, including chemotherapy.
- The location of the cancer: The location of the cancer within the cervix and whether it has spread to nearby tissues or organs affect treatment planning. Cervical cancers located closer to the outer surface of the cervix may be more accessible for surgical removal, while those deeper within the tissue may require additional treatments like radiation therapy or chemotherapy.
- Whether the cancer has spread: The extent of cancer spread, known as staging, determines the appropriate treatment approach. Cervical cancer that has spread beyond the cervix may require more aggressive treatment, such as chemotherapy or targeted therapy, to address metastases in other parts of the body.
-
The general health of the person: The overall health and medical history of the individual play a crucial role in determining the most suitable treatment options. Factors such as age, presence of other medical conditions, and treatment tolerance influence treatment decisions and may impact treatment outcomes.
Treatment options include:
These are treatment options for cervical cancer:
- Surgery to remove the cancer cells or infected body parts: Surgical procedures may involve removing the cancerous cells or infected parts of the cervix, uterus (womb), or surrounding tissues. The extent of surgery depends on the stage and location of the cancer. Examples include cone biopsy, radical hysterectomy, or pelvic exenteration.
- Radiation therapy: Radiation therapy uses high-energy beams to target and destroy cancer cells. It can be delivered externally (external beam radiation) or internally (brachytherapy). Radiation therapy may be used alone or in combination with other treatments like surgery or chemotherapy.
- Chemotherapy: Chemotherapy involves the use of drugs, either injected into the bloodstream or taken orally, to kill cancer cells or prevent their growth and spread. Chemotherapy is often used in combination with surgery or radiation therapy for advanced or recurrent cervical cancer.
- Targeted therapy: Targeted therapy targets specific molecules or pathways involved in cancer cell growth and survival. These drugs can block the growth and spread of cancer cells while minimizing damage to healthy cells. Targeted therapy may be used in combination with other treatments for advanced or recurrent cervical cancer.
-
Immunotherapy: Immunotherapy works by stimulating the body’s immune system to recognize and attack cancer cells. These medications can help the immune system better target and destroy cancer cells, potentially leading to better treatment outcomes. Immunotherapy may be used alone or in combination with other treatments for advanced cervical cancer.
Different surgeries involve removing:
These are different types of surgeries for cervical cancer:
- Cervical conization or cone biopsy: This surgery involves removing a cone-shaped piece of tissue from the cervix. It is typically performed when the cancer is very small or in situ (confined to the surface layers of the cervix). This procedure aims to remove the abnormal cells while preserving the rest of the cervix for future fertility.
- Radical trachelectomy: In this surgery, the cervix and upper part of the vagina are removed, but the uterus (womb) is preserved. This procedure is offered to women with early-stage cervical cancer who wish to preserve their fertility and have the potential to become pregnant in the future.
- Hysterectomy: A hysterectomy involves the removal of the cervix and uterus. Depending on the extent of the disease and individual factors, additional structures such as the ovaries and fallopian tubes may also be removed. This surgery is commonly recommended for more advanced stages of cervical cancer or when fertility preservation is not a concern.
- Pelvic exenteration: This extensive surgery is reserved for cases where cervical cancer has recurred or spread extensively to nearby organs and tissues. It involves removing the cervix, uterus, ovaries, fallopian tubes, and potentially parts of the bladder, bowel, vagina, or rectum. Pelvic exenteration aims to achieve complete removal of cancerous tissue but can have significant effects on urinary, bowel, and sexual function.
The choice of surgery depends on factors such as the stage and extent of cervical cancer, the patient’s desire for fertility preservation, and their overall health. Surgical options are often discussed with a gynecologic oncologist, who specializes in the treatment of gynecologic cancers, to determine the most appropriate approach for each individual case.

Guidelines for cancer screening
Regardless of sexual history, every woman beginning at age 21 years should be screened for cancer
Every woman between the ages 21 to 29 years of age should receive a pap test every 3 years
Every woman 30 years and older should have co-testing with Pap and HPV every five years, or Pap test alone every three years
Women with no history of cervical cancer do not require a routine pap test
All women who had total hysterectomy (removal of the womb and cervix) for mild conditions do not require routine pap tests
Screening for cervical cancer can be stopped at 65 years if the woman had 3 or more normal consecutive pap tests and no abnormal tests within the last 20 years
Women who were treated for a neoplasm (abnormal growth) of the cervix are required to continue screening for cancer for 20 years
All women with weakened immune systems such as HIV infection, history of cervical cancer should continue screening as recommended by their healthcare provider.
WHEN TO SEEK URGENT MEDICAL CARE
It’s essential to seek urgent medical care if you experience any of the following symptoms related to cervical cancer or other gynecological issues:
- Heavy, watery, or bloody vaginal discharge: Unusual vaginal discharge, especially if it is heavy, watery, or bloody, could indicate various gynecological conditions, including cervical cancer.
- Offensive discharge: Foul-smelling vaginal discharge may be a sign of infection or other underlying issues that require medical attention.
- Vaginal bleeding after intercourse, between menstrual periods, or after menopause: Any unexplained vaginal bleeding, particularly after intercourse, between periods, or after menopause, should be evaluated by a healthcare provider.
- Heavy menstrual periods: Excessively heavy or prolonged menstrual bleeding, also known as menorrhagia, can be a symptom of various gynecological conditions, including cervical cancer.
- Pelvic pain or discomfort: Persistent pelvic pain or discomfort, especially if it is severe or worsening over time, should prompt medical evaluation to determine the underlying cause.
- Changes in bowel or bladder habits: Any changes in bowel or bladder habits, such as difficulty urinating, blood in the urine or stool, or changes in bowel movements, should be assessed by a healthcare provider.
- Unexplained weight loss or fatigue: Unintentional weight loss, especially when accompanied by fatigue or weakness, may be a sign of an underlying health issue that requires investigation.
- Pain or bleeding during or after sexual intercourse: Pain or bleeding during or after sexual intercourse, known as dyspareunia, may indicate various gynecological problems, including cervical cancer.
If you experience any of these symptoms, it’s important to seek prompt medical attention from a healthcare provider or gynecologist. Early detection and intervention can lead to better outcomes and improve the effectiveness of treatment. Don’t hesitate to contact your healthcare provider if you have any concerns or questions about your gynecological health.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

