Asthma Management 101: Triggers, Medications, and Lifestyle Changes
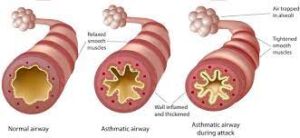
An incurable disease where the muscles around the lungs tighten due to the swelling of lining around the lungs. The person encounters difficulty breathing as an excessive amount of mucus builds up in the lungs. In other words, asthma is a chronic respiratory condition that affects the airways, causing them to become inflamed, swollen, and narrowed. Asthma can cause both minor and severe health issues such as having difficulty sleeping or participating in physical activities. Severe cases can lead to hospitalization or even death if not managed properly. Early diagnosis and treatment are key to managing and controlling asthma symptoms so those affected can continue living healthy lives. Please keep reading for details on the following topics:
Symptoms of asthma
Triggers of Asthma
Consequences of asthma
How asthma is diagnosed
How to manage asthma
Natural remedies to soothe asthma
Best foods for asthma
Asthma medication
If someone is having an asthma attack
When to seek urgent medical care
Warnings
Symptoms of asthma
Symptoms vary from person to person and can range from mild to severe. Common symptoms include:
- Wheezing: A whistling or squeaky sound when breathing, often heard during exhalation.
- Chest tightness: A sensation of pressure or constriction in the chest, which may feel like someone is squeezing or sitting on your chest.
- Difficulty breathing: Feeling short of breath or having trouble catching your breath, especially during physical activity or when exposed to triggers.
- Bluish color to the nails and skin: Also known as cyanosis, this occurs when oxygen levels in the blood are low, leading to a bluish tint in the skin, lips, or nails.
- Coughing: A persistent cough, particularly at night or early in the morning, which may worsen with exercise or exposure to triggers.
- Difficulty talking: Feeling out of breath or unable to speak in full sentences due to breathing difficulties.
- Anxiety: Feeling anxious or panicky, often in response to difficulty breathing.
- Tiredness: Feeling fatigued or exhausted, especially during or after an asthma flare-up.
- Chest pain: Discomfort or pressure in the chest, which may be mistaken for a heart attack in some cases.
- Rapid breathing: Breathing at a faster rate than normal, often as a result of trying to compensate for difficulty breathing.
- Hyperventilation: Breathing excessively fast and shallow, leading to decreased levels of carbon dioxide in the blood.
- A whistling sound when inhaling or exhaling: Similar to wheezing, this may occur during breathing and is often a sign of narrowed airways.
- Seesaw motions in the chest: Visible movements of the chest wall during breathing, indicating increased effort to breathe.
-
Tight neck and chest muscles: Feeling tension or tightness in the muscles of the neck and chest, often as a result of difficulty breathing.
Triggers of Asthma
Triggers are substances, activities, or environmental factors that can worsen symptoms or lead to asthma attacks. Common triggers include:
- Allergens: Substances that can cause allergic reactions, such as pollen, dust mites, mold, pet dander, and cockroach droppings.
- Respiratory infections: Viral infections, such as the common cold or flu, can inflame the airways and trigger asthma symptoms.
- Exercise: Physical activity, particularly in cold or dry air, can lead to shortness of breath, coughing, and wheezing in people with exercise-induced asthma.
- Tobacco smoke: Both firsthand and secondhand smoke can irritate the airways and trigger symptoms.
- Air pollution: Outdoor pollutants, such as vehicle exhaust, industrial emissions, and particulate matter, can worsen symptoms, especially in urban areas with poor air quality.
- Strong odors and fumes: Irritating smells from perfumes, cleaning products, paints, and chemicals can trigger asthma symptoms in sensitive individuals.
- Weather changes: Cold air, humidity, thunderstorms, and sudden changes in temperature or barometric pressure can exacerbate asthma symptoms.
- Dust and dust mites: Dust particles and dust mite allergens found in bedding, carpets, and upholstered furniture can trigger symptoms, particularly when disturbed.
- Cockroach allergens: Proteins found in cockroach saliva, droppings, and body parts can trigger allergic reactions and worsen symptoms.
- Mold: Indoor and outdoor mold spores can trigger symptoms, especially in damp or humid environments.
- Pet allergens: Proteins found in the skin, saliva, and urine of pets can trigger allergic reactions and worsen symptoms in pet-sensitive individuals.
- Pollutants: Indoor pollutants, such as volatile organic compounds (VOCs), formaldehyde, and indoor combustion byproducts, can worsen asthma symptoms when present in high concentrations.
- Strong emotions: Stress, anxiety, and strong emotions can trigger symptoms in some individuals.
- Medications: Certain medications, such as aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), and beta-blockers, can trigger symptoms or exacerbate existing asthma.
-
Occupational exposures: Workplace irritants, such as chemicals, dust, fumes, or allergens, can trigger occupational asthma in susceptible individuals.
Consequences of asthma can have various consequences, both immediate and long-term, on an individual’s health and quality of life. Some of the consequences include:
- Acute asthma attacks: can lead to sudden and intense symptoms, including severe shortness of breath, wheezing, coughing, and chest tightness. Without prompt medical treatment, asthma attacks can be life-threatening.
- Hospitalization: for intensive treatment, including oxygen therapy, bronchodilator medications, corticosteroids, and monitoring for complications such as respiratory failure.
- Decreased lung function: Long-term inflammation and remodeling of the airways in asthma can lead to a gradual decline in lung function over time. This can result in reduced lung capacity, impaired exercise tolerance, and increased susceptibility to respiratory infections.
- Limitations on physical activity: Asthma symptoms such as shortness of breath, wheezing, and chest tightness can restrict an individual’s ability to participate in physical activities, leading to reduced fitness levels and decreased quality of life.
- Sleep disturbances: Nighttime asthma symptoms, including coughing, wheezing, and difficulty breathing, can disrupt sleep patterns and lead to sleep deprivation, fatigue, and daytime drowsiness.
- Psychological impact: Living with asthma can have psychological consequences, including anxiety, depression, stress, and feelings of frustration or helplessness due to the unpredictability of asthma symptoms and the need for ongoing management.
- Missed school or work: Asthma exacerbations and medical appointments may result in missed days of school or work, leading to academic or occupational challenges, decreased productivity, and financial strain.
- Medication side effects: Some medications, particularly oral corticosteroids used to control inflammation during exacerbations, may cause side effects such as weight gain, mood changes, insomnia, osteoporosis, and increased susceptibility to infections.
- Impact on oral health: Long-term use of asthma medications, particularly inhaled corticosteroids, can increase the risk of oral health problems such as dental caries, gingivitis, and oral thrush (candidiasis).
-
Social and lifestyle limitations: Asthma symptoms and the need for ongoing management may impact social activities, travel plans, and lifestyle choices, leading to feelings of isolation, frustration, and reduced quality of life.
How asthma is diagnosed

Diagnosis typically involves a combination of medical history, physical examination, lung function tests, and other diagnostic procedures. Here’s an overview of the diagnostic process for asthma:
- Medical history: The healthcare provider will ask detailed questions about the individual’s symptoms, including the frequency, duration, and severity of coughing, wheezing, shortness of breath, and chest tightness. They will also inquire about any triggers that worsen or alleviate symptoms, past medical history, family history of asthma or other respiratory conditions, and medication use.
- Physical examination: The healthcare provider will perform a physical examination, which may include listening to the lungs with a stethoscope to detect wheezing or other abnormal sounds, examining the nose and throat for signs of allergies or nasal congestion, and assessing overall respiratory function.
- Lung function tests: Pulmonary function tests (PFTs) are essential for diagnosing and monitoring asthma. The most common lung function test used to diagnose asthma is spirometry, which measures how much air an individual can exhale and how quickly they can exhale it. Spirometry can assess lung function before and after bronchodilator medication administration to determine if airflow obstruction improves with treatment.
- Peak expiratory flow (PEF) measurement: PEF monitoring involves using a handheld device called a peak flow meter to measure the maximum airflow that can be exhaled forcefully in one breath. Regular monitoring of PEF at home can help identify patterns of airflow variability and assess asthma control.
- Methacholine challenge test: In cases where spirometry results are inconclusive, a methacholine challenge test may be performed. This test involves inhaling increasing concentrations of methacholine, a medication that causes temporary narrowing of the airways. If the airways narrow significantly in response to methacholine, it indicates airway hyperresponsiveness, a characteristic feature of asthma.
- Fractional exhaled nitric oxide (FeNO) test: This noninvasive test measures the level of nitric oxide in exhaled breath, which is elevated in individuals with eosinophilic airway inflammation, a common feature of allergic asthma. Elevated FeNO levels may indicate ongoing airway inflammation and help guide asthma management decisions.
- Chest X-ray or imaging studies: Although not routinely performed for asthma diagnosis, chest X-rays or imaging studies may be ordered to rule out other respiratory conditions that mimic asthma symptoms, such as pneumonia, bronchitis, or pulmonary embolism.
- Allergy testing: Allergy skin tests or blood tests (specific IgE tests) may be recommended to identify specific allergens that trigger symptoms, particularly in individuals with allergic asthma.
-
Other tests: Additional tests, such as sputum eosinophil count, allergy testing, or exhaled breath condensate analysis, may be considered in specific clinical scenarios or research settings to further characterize airway inflammation and guide treatment decisions.
How to manage asthma

Management involves a combination of medications, lifestyle modifications, and ongoing monitoring to achieve optimal asthma control and minimize the risk of exacerbations. Here are key strategies for managing asthma:
- Medications:
- Controller medications: These medications are taken regularly to control underlying inflammation and prevent asthma symptoms. They include inhaled Bronchodilators- (Salbutamol or Ventolin), Corticosteroids (to ease the inflammation), long-acting beta-agonists, leukotriene modifiers, and biologic therapies (e.g., omalizumab, mepolizumab).
- Quick-relief medications: Also known as rescue or reliever medications, these medications provide rapid relief of symptoms during acute exacerbations. They include short-acting beta-agonists (e.g., albuterol) and oral corticosteroids (e.g., prednisone) for severe exacerbations.
- Identifying and avoiding triggers:
- Identify and minimize exposure to allergens that trigger asthma symptoms, such as pollen, dust mites, pet dander, mold, and cockroach allergens.
- Avoid exposure to irritants such as tobacco smoke, air pollution, strong odors, perfumes, and chemical fumes.
- Take precautions during extreme weather conditions, such as cold air or high humidity, which can trigger asthma symptoms.
- Developing an asthma action plan:
- Work with a healthcare provider to develop a personalized asthma action plan that outlines daily medications, steps to take during asthma exacerbations, and when to seek medical help.
- The asthma action plan should include instructions for monitoring symptoms, adjusting medications, using peak flow meters, and recognizing signs of worsening asthma.
- Regular monitoring:
- Monitor symptoms, peak expiratory flow rates, and medication use regularly to assess asthma control and adjust treatment as needed.
- Keep track of asthma triggers, symptoms, medication adherence, and peak flow measurements in a written or electronic asthma diary.
- Maintaining a healthy lifestyle:
- Engage in physical activities that promote cardiovascular fitness and lung function, such as walking, swimming, or cycling. Warm up before exercising and use asthma medications as prescribed to prevent exercise-induced asthma.
- Consume a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats to support overall health and immune function.
- Obesity is associated with worse asthma control and increased risk of asthma exacerbations. Aim to achieve and maintain a healthy weight through diet and regular exercise.
- Avoid tobacco smoke exposure, including secondhand smoke, as it can worsen asthma symptoms and increase the risk of asthma exacerbations.
- Managing comorbid conditions:
- Address comorbid conditions that may worsen asthma control, such as allergic rhinitis, sinusitis, gastroesophageal reflux disease (GERD), obstructive sleep apnea, and obesity.
- Work with healthcare providers to manage these conditions effectively and optimize asthma control.
- Education and support:
- Educate yourself and your caregivers about asthma, including symptoms, triggers, medications, and self-management techniques.
- Join support groups or educational programs to connect with others living with asthma, share experiences, and learn coping strategies.
-
Regular follow-up with healthcare providers:
- Schedule regular follow-up appointments with healthcare providers to assess asthma control, review treatment plans, adjust medications as needed, and address any concerns or questions.
- Be proactive in discussing any changes in asthma symptoms, medication side effects, or triggers with your healthcare team.
- Natural remedies to soothe the symptoms of asthma:
-
- Ginger contains compounds that have anti-inflammatory properties, which can help to reduce airway inflammation and improve breathing.
- Another natural remedy is honey, which can be added to tea or warm water to help soothe the throat and reduce coughing.
- Eucalyptus oil has been shown to have a relaxing effect on the airways and may help to improve breathing.
- caffeine– helps relax the bronchial tubes, thus improve breathing
- carotenoids– give foods their yellow, orange and red color. They are found in foods such as apricots, carrots, cantaloupe, sweet potatoes, apples and tomatoes.
- vitamin C– antioxidants such as citrus fruits, onions,
- vitamin E– vegetable oils, tomatoes, sweet potatoes, sunflower seeds, fruits, vegetables, soya bean, grains. Vitamin E is also an antioxidant that protects the body from free radicals
- vitamin D– can be obtained from the sunlight
- magnesium– spinach, avocados, legumes, oysters
- selenium– a mineral essential in stopping lung inflammation. enriched grains, walnuts, tuna, beef
- parsley– antioxidant. can be used in soups, salads, stews to help improve breathing
- rosemary– antioxidant, antispasmodic can be ingested as a tea or food seasoning
- ginkgo biloba– (do not take with any anticoagulant such as aspirin, warfarin because it can increase the bleeding time.
- Boswellia serrata– is a tree-bark that has anti-inflammatory properties to help reduce the number of asthma attacks
It’s important to note that while natural remedies can be helpful, they should never be used in place of prescribed medication or medical advice.
-
- deep breathing exercises-can be a useful tool in controlling symptoms and improving overall lung function. By practicing regular deep breathing exercises, individuals can increase their lung capacity and reduce the frequency and severity of asthma attacks. These exercises involve taking slow, controlled breaths in through the nose and out through the mouth, focusing on expanding the lungs fully and engaging the diaphragm. It is recommended to practice these exercises daily, especially during times of stress or when experiencing symptoms. However, it is important to consult with a healthcare professional before beginning any new exercise regimen, particularly if you are experiencing severe symptoms.
-
- yoga and meditation: have been found to be effective in controlling symptoms. Breathing techniques practiced in yoga can improve lung capacity and reduce the frequency and severity of asthma attacks. Meditation, on the other hand, can help people with asthma manage stress, which is a known trigger for asthma.
If someone is having an asthma attack, it’s crucial to take prompt action to help alleviate their symptoms and prevent the situation from worsening. Here are steps to follow if someone is experiencing an attack:

- Stay Calm: Remain calm and reassure the person experiencing the attack. Panic can worsen symptoms and make it harder for them to breathe.
- Assist the Person: Help the person sit up straight in a comfortable position, preferably in an upright position. This can help ease breathing by allowing the airways to expand more fully.
- Encourage Slow Breathing: Encourage the person to take slow, deep breaths. Breathing exercises can help them relax and control their breathing. Instruct them to inhale slowly through the nose and exhale slowly through pursed lips.
- Administer Quick-Relief Medication: If the person has a quick-relief inhaler (usually a short-acting beta-agonist like albuterol), assist them in using it as prescribed. Follow the instructions on the inhaler or asthma action plan. Typically, this involves shaking the inhaler, having the person exhale fully, then inhaling the medication deeply into the lungs. Repeat as necessary, following the prescribed dosage.
- Stay with the Person: Stay with the person and monitor their condition closely. If symptoms persist or worsen despite using the inhaler, seek emergency medical assistance immediately.
- Call for Emergency Help: If the person’s symptoms do not improve after using their inhaler, if they are struggling to breathe, if their lips or nails turn blue, or if they become unresponsive, call emergency services immediately. Time is of the essence in severe asthma attacks, and prompt medical intervention is essential.
- Provide Comfort: Offer reassurance and comfort to the person experiencing the asthma attack. Stay by their side, offer words of encouragement, and let them know that help is on the way.
-
Continue to Monitor: Even if the person’s symptoms improve after using the inhaler, continue to monitor them closely. Some attacks may require additional medical treatment, and it’s essential to remain vigilant until help arrives.
When to seek urgent medical care
Knowing when to seek urgent medical care for asthma is essential for managing the condition and preventing potentially life-threatening complications. Here are situations that warrant immediate medical attention:
- Severe Difficulty Breathing: If the person with asthma is experiencing severe difficulty breathing, gasping for air, or struggling to speak due to shortness of breath, seek urgent medical care immediately.
- Blue Lips or Fingernails: Bluish discoloration of the lips, fingernails, or skin (cyanosis) indicates a severe lack of oxygen in the blood and requires immediate medical attention.
- Confusion or Altered Mental Status: Confusion, disorientation, or altered mental status can be signs of inadequate oxygen delivery to the brain and should prompt a call for emergency medical assistance.
- Persistent Wheezing or Coughing: If the person’s wheezing or coughing persists despite using their rescue inhaler, it may indicate inadequate asthma control or a severe exacerbation requiring medical intervention.
- No Improvement After Using Inhaler: If the person’s symptoms do not improve after using their quick-relief inhaler (e.g., albuterol) as prescribed, seek emergency medical assistance immediately.
- Inability to Perform Daily Activities: If symptoms prevent the person from performing daily activities, such as walking or talking, or if they are unable to complete sentences due to shortness of breath, seek urgent medical care.
- Peak Flow Measurements: If the person measures their peak expiratory flow rate (PEFR) using a peak flow meter and the reading is in the red zone (signifying severe airflow limitation), seek urgent medical attention.
- Persistent Chest Pain: Chest pain or tightness that persists despite using asthma medication may indicate a more severe asthma exacerbation or a potential heart-related issue requiring immediate medical evaluation.
- Use of Accessory Muscles: If the person is using their neck or chest muscles to breathe (retractions) or if there is visible neck or chest movement with each breath, it suggests severe respiratory distress and necessitates urgent medical care.
- Previous History of Severe Asthma Attacks: If the person has a history of severe asthma attacks requiring hospitalization or intensive care unit (ICU) admission, any exacerbation of symptoms should prompt immediate medical attention.
In any of these situations, it’s essential to act quickly and seek emergency medical assistance by calling emergency services or going to the nearest emergency department. Time is critical in severe asthma attacks, and prompt medical intervention can be life-saving.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

