Managing Group B Strep: How It Affects Newborns and What You Can Do
Group B Streptococcus (GBS) is a serious infection caused by type of bacterium that accumulates in the human body, most commonly in the vagina, intestines or rectum. It is estimated that about 30-35% of women have GBS in their bodies, and it can be transferred to the baby during delivery. GBS can cause serious health problems for newborns if left untreated, including pneumonia, meningitis, sepsis and even death. While GBS infection is treatable with antibiotics, prevention is key. All pregnant women should receive screening and immunization to reduce the risks associated with GBS infection in babies. Please keep reading for details on the following topics:
Definition of Group B Streptococcal infection
Manifestations of Group B Streptococcal infection
Diagnosis Group B Streptococcal infection
TRANSMISSION OF GROUP B STREPTOCOCCAL INFECTION
From a pregnant woman to her baby during delivery
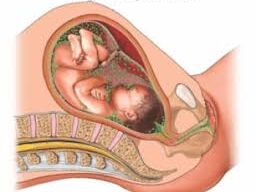 How infections are transmitted to the fetus
How infections are transmitted to the fetus
Risk Factors for GBS Infection:
- Previous baby with a GBS infection.
- Premature birth (before 37 weeks of gestation).
- Prolonged rupture of membranes (water breaking more than 18 hours before delivery).
- Developing a fever during labor.
- Urinary tract infections caused by GBS during the current pregnancy.
MANIFESTATIONS OF GROUP B STREPTOCOCCAL INFECTION
Hypothermia (low temperature)
Rapid breathing
Difficulty eating
Sepsis (infection in the blood)
Pneumonia (infection in the lungs)
Meningitis (infection in the brain and spinal cord)
Newborns with GBS infection may show signs of:
- Early-onset infection (within the first week of life): This can include respiratory distress, fever, lethargy, poor feeding, and difficulty breathing.
- Late-onset infection (1 week to several months after birth): This can include meningitis, poor feeding, and irritability.
DIAGNOSIS OF GROUP B STREPTOCOCCAL INFECTION
The diagnosis of Group B Streptococcal (GBS) infection typically involves testing during pregnancy, as GBS is often present in the vagina or rectum without causing symptoms in the mother. The key steps in diagnosing a GBS infection are:
1. Screening for GBS in Pregnant Women:
Pregnant women are routinely screened for GBS between the 35th and 37th weeks of pregnancy. The screening involves taking swabs from the vagina and rectum to test for the presence of the bacteria.
- Procedure:
- A sterile swab is inserted into the vagina and rectum to collect samples.
- The samples are then cultured (grown in a lab) for 48 hours to check for the presence of the bacteria.
Lab testing: The swabs are sent to a laboratory where they are cultured to detect the presence of Group B Streptococcus bacteria.
- Positive result: If GBS is detected in the culture, the woman is considered colonized with GBS, but this does not necessarily mean she will develop an infection. However, it does mean that there is a risk of passing the bacteria to the baby during labor.
2. Risk-Based Screening:
Some women may be assessed based on risk factors rather than routine screening. This is less common but may apply to specific situations, such as:
- Previous baby with a GBS infection.
- Premature rupture of membranes.
- Prolonged labor.
- Fever during labor.
For these women, antibiotics are typically given during labor to reduce the risk of transmission to the baby, even if they have not undergone routine screening.
3. Diagnosis of GBS Infection in Newborns:
Newborns can be diagnosed with GBS infection based on clinical signs and laboratory tests:
- Symptoms: Symptoms of GBS infection in a newborn can develop within the first few days after birth and include fever, difficulty breathing, lethargy, poor feeding, irritability, or respiratory distress, diagnostic tests are performed:
- Blood culture: A sample of the baby’s blood is taken and cultured to check for the presence of GBS bacteria.
- CSF (Cerebrospinal Fluid) culture: If the baby has signs of meningitis (e.g., fever, irritability, lethargy), a sample of cerebrospinal fluid (CSF) may be collected via a lumbar puncture to test for GBS.
- Chest X-ray: If pneumonia is suspected, an X-ray may be done to check for lung infection.
- Urine culture: A urine sample can be tested for a urinary tract infection caused by GBS.
- Testing for Neonatal Infections: If an infant exhibits signs of infection, doctors may also order chest X-rays or lumbar puncture (spinal tap) to look for pneumonia or meningitis, respectively.
Diagnosis of Active Infection in the mother:
In addition to the screening swab test, the diagnosis of GBS infection in a pregnant woman is made based on clinical signs and symptoms, as well as bacterial cultures:
- Urinary tract infections (UTIs) caused by GBS: A urine sample is taken to test for the bacteria if a woman shows symptoms such as pain or burning during urination or fever during pregnancy.
- Endometritis (infection of the uterine lining): After childbirth or cesarean section, GBS can cause uterine infections, leading to fever, pain, and other signs of infection.
- Wound infection: If a woman has an infection at the site of a cesarean incision, GBS can be cultured from the wound.
Risks and Complications:
- Neonatal Infections: The primary risk associated with GBS during pregnancy is the potential for the baby to develop infections, which can include:
- Sepsis: A severe, widespread infection in the bloodstream.
- Pneumonia: Infection of the lungs.
- Meningitis: Inflammation of the membranes around the brain and spinal cord.
- Stillbirth: In rare cases, GBS can lead to stillbirth or miscarriage if left untreated.
- Maternal Infections: GBS can also cause infections in pregnant women, although it is less common. These include urinary tract infections (UTIs), endometritis (infection of the uterine lining), and wound infections after a cesarean section.
Screening and Prevention:
- Screening: Pregnant women are typically screened for GBS between the 35th and 37th week of pregnancy. This is done by taking a swab from the vagina and rectum to test for the presence of the bacteria.
- Treatment: If a woman tests positive for GBS or has risk factors (e.g., previous GBS-infected newborn, premature labor, fever during labor), antibiotics (usually penicillin) are administered intravenously during labor to prevent transmission to the baby. This is effective in reducing the risk of neonatal infection.
- Alternative antibiotics: If a woman is allergic to penicillin, other antibiotics, such as clindamycin or erythromycin, may be used.
HOW GROUP B STREPTOCOCCOL INFECTION IS TREATED
Antibiotics given to infected women during labor
Antibiotics given to babies after birth
Fluids to infected babies
Oxygen given to infected babies who are very ill
Treatment (If diagnosed):
If a GBS infection is diagnosed in a newborn, the baby will be treated with intravenous antibiotics (often penicillin or ampicillin) to combat the infection. The sooner the treatment is started, the better the outcomes for the baby.
Importance of Antibiotic Prophylaxis:
Administering antibiotics during labor is the most effective way to prevent GBS infections in newborns. This is especially important in preventing early-onset GBS disease, which can occur within the first week of life.
Neonatal Care:
If a baby shows signs of a GBS infection after birth (such as difficulty breathing, fever, or lethargy), they are immediately tested and treated with antibiotics.
Routine screening and treatment have significantly reduced the incidence of GBS-related neonatal infections, but it remains an important aspect of prenatal care to ensure the health of both mother and baby.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.

