Understanding Neuropathy Causes, Symptoms, and Treatment Options
Neuropathy, a condition characterized by nerve damage, has become a prevalent concern for many. Whether stemming from causes like diabetic neuropathy or chemotherapy-induced neuropathy, understanding its intricacies is vital for effective management and treatment.

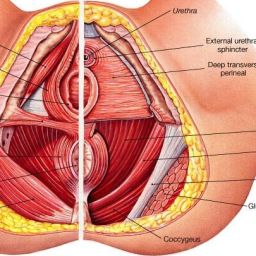
Neuropathy, also known as peripheral neuropathy, is a medical condition that involves damage or dysfunction of the peripheral nerves, which are the nerves outside the brain and spinal cord. These nerves are responsible for transmitting signals between the central nervous system (the brain and spinal cord) and the rest of the body, including the limbs, organs, and skin.
Neuropathy can result from a variety of causes, and it can affect one nerve (mononeuropathy), multiple nerves in different areas (multiple mononeuropathy), or many nerves simultaneously (polyneuropathy). The condition can be acute (short-term) or chronic (long-term).
Common causes of neuropathy include:
- Diabetes: Diabetes is one of the most common causes of neuropathy, known as diabetic neuropathy. Prolonged high blood sugar levels can lead to nerve damage. It’s believed that the excess sugar in the blood disrupts the normal functioning of nerves and their protective coverings. High blood sugar levels can directly damage nerve fibers and impair blood flow to the nerves. This causes them to become less efficient at transmitting signals, leading to neuropathic symptoms. Effective management of diabetic neuropathy involves maintaining optimal blood sugar control. Keeping blood sugar levels within a healthy range can slow or even prevent further nerve damage.
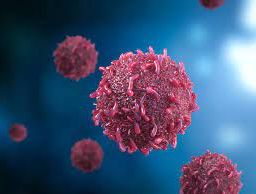
- Chemotherapy: Chemotherapy-induced neuropathy (CIPN) is a common side effect of certain cancer treatments, including chemotherapy drugs. These drugs can be toxic to nerves, leading to damage. The exact mechanism is complex and can vary depending on the specific drug. However, many chemotherapy drugs disrupt the normal functioning of nerve cells, impairing their ability to transmit signals. Management of CIPN may involve adjusting chemotherapy protocols, reducing drug dosages, or using medications to alleviate symptoms. In some cases, CIPN can be a limiting factor in cancer treatment, and balancing the benefits and risks of chemotherapy is crucial.
- Infections: Certain infections, such as shingles (varicella-zoster virus), HIV, Lyme disease, and hepatitis C, can lead to neuropathy. The infections themselves or the body’s immune response to them can damage nerves. In some cases, the virus directly attacks and damages nerves. In other cases, the body’s immune system mistakenly targets nerve tissue, causing inflammation and damage. Effective management of infectious neuropathy often involves treating the underlying infection with antiviral medications or antibiotics. Managing the infection can help prevent further nerve damage.
- Autoimmune Diseases: Autoimmune diseases like Guillain-Barré syndrome, lupus, and rheumatoid arthritis can trigger neuropathy. In these conditions, the immune system mistakenly attacks the body’s own tissues, including nerves. The immune system’s attack on nerve tissue causes inflammation and damage, leading to neuropathic symptoms. Management of autoimmune-related neuropathies often requires immunosuppressive medications to reduce the immune system’s attack on nerves. Treating the underlying autoimmune condition is essential to prevent further damage.
- Trauma or Injury: Physical injuries or trauma to nerves can cause neuropathy.
- Alcohol Abuse: Excessive alcohol consumption can lead to alcoholic neuropathy.
- Toxins and Medications: Exposure to certain toxins or medications can damage nerves.
- Genetics: Some forms of neuropathy can be hereditary.
Now let’s explore different types of neuropathy and the role of nerves in sensory and motor functions:
- Diabetic Neuropathy:
- Role of Nerves: In diabetic neuropathy, high blood sugar levels over an extended period damage the nerves, primarily affecting the peripheral nervous system. These nerves transmit information between the central nervous system (the brain and spinal cord) and the extremities and organs.
- Impact on Sensory and Motor Functions: Diabetic neuropathy can lead to various sensory symptoms, including numbness, tingling, and burning pain in the feet and hands. Motor functions may be affected, resulting in muscle weakness and poor coordination. These symptoms can make activities like walking, buttoning a shirt, and balance maintenance challenging.
- Chemotherapy-Induced Neuropathy (CIPN):
- Role of Nerves: Chemotherapy-induced neuropathy is a side effect of certain cancer treatments. Chemotherapy drugs can damage the nerves, disrupting their ability to send signals properly.
- Impact on Sensory and Motor Functions: CIPN primarily affects sensory functions. Patients may experience tingling, numbness, or pain in their hands and feet. This can hinder fine motor skills, making tasks like writing or picking up small objects difficult. In severe cases, it can affect balance and coordination.
- Peripheral Neuropathy:
- Role of Nerves: Peripheral neuropathy is a broad term encompassing various nerve disorders affecting the peripheral nerves throughout the body.
- Impact on Sensory and Motor Functions: The symptoms of peripheral neuropathy can vary widely depending on the nerves affected and the underlying cause. They may include numbness, tingling, muscle weakness, and difficulty with balance and coordination. This condition can disrupt both sensory and motor functions, making it challenging to perform daily activities.
- Autonomic Neuropathy:
- Role of Nerves: Autonomic neuropathy affects the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, and blood pressure.
- Impact on Sensory and Motor Functions: Autonomic neuropathy primarily impacts autonomic functions rather than sensory and motor functions. It can lead to issues like dizziness, heart rate irregularities, digestive problems, and changes in sweating patterns.
- Hereditary Neuropathies:
- Role of Nerves: Hereditary neuropathies are genetic disorders that affect the peripheral nerves.
- Impact on Sensory and Motor Functions: These conditions can lead to a range of symptoms, such as muscle weakness, loss of sensation, and impaired coordination. The specific symptoms can vary depending on the type of hereditary neuropathy.
- Idiopathic Neuropathy:
- Role of Nerves: Idiopathic neuropathy refers to cases where the cause of nerve damage is unknown.
- Impact on Sensory and Motor Functions: Like other types of neuropathy, idiopathic neuropathy can result in sensory and motor symptoms, including numbness, tingling, pain, muscle weakness, and coordination problems.

Neuropathy can cause a wide range of symptoms, which can vary depending on the type of neuropathy and the nerves affected. Common symptoms of neuropathy include:
- Numbness or Tingling: Many people with neuropathy experience a sensation of numbness or tingling in their extremities, such as the hands and feet.
- Burning or Electric Shock-Like Pain: Neuropathy often causes a burning or electric shock-like pain, which can be constant or intermittent.
- Muscle Weakness: Weakness in the muscles, particularly in the affected area, is a common symptom.
- Sensitivity to Touch: Some people with neuropathy become hypersensitive to touch and may find even light touch painful.
- Loss of Coordination: Neuropathy can lead to a loss of coordination and balance, increasing the risk of falls.
- Muscle Cramps or Spasms: Cramps and muscle spasms may occur in the affected areas.
- Changes in Sensation: Neuropathy can result in unusual sensations, such as a feeling of “pins and needles” or a sense of fullness or swelling in the affected area.
- Temperature Sensitivity: Some individuals with neuropathy experience sensitivity to temperature changes, finding cold or heat uncomfortable.
- Loss of Reflexes: Reflexes may be reduced or absent in the affected limbs.
- Difficulty with Fine Motor Skills: Tasks that require fine motor skills, such as buttoning a shirt or picking up small objects, may become more challenging.
- Autonomic Symptoms: In some cases, autonomic nerves can be affected, leading to symptoms like dizziness, changes in blood pressure, digestive issues, and changes in sweating.
- Pain Disruption of Sleep: Neuropathic pain can interfere with sleep, causing sleep disturbances and fatigue.
Diagnostic process for neuropathy, including the essential steps involved:
I. Medical History
- Patient Interview: This is conducted to obtain a detailed medical history from the patient. This includes questions about their symptoms, their onset and progression, and any relevant family history. Underlying medical conditions such as diabetes, cancer, autoimmune diseases, or recent infections, may be associated with neuropathy. All medications the patient is taking must be identified, as some drugs can cause or exacerbate neuropathy.

II. Physical Examination
- Neurological Examination: A comprehensive neurological examination is conducted to assess sensory and motor functions. This may include:
- Testing for changes in sensation, such as numbness, tingling, and hypersensitivity.
- Assessing muscle strength and coordination.
- Checking for reflexes, as neuropathy can affect reflex responses.
- Skin and Foot Examination: In cases of peripheral neuropathy, the skin and feet are inspected for any wounds, sores, or ulcers, as patients with reduced sensation may be at risk of injury without realizing it.
- Blood Tests: Several blood tests may be conducted to identify the underlying cause or contributing factors. This may include:
- Blood glucose levels for diabetes assessment.
- Complete blood count (CBC) to check for infections.
- Antibody tests for autoimmune conditions.
- Vitamin B12 levels, as a deficiency can lead to neuropathy.
- Nerve Function Tests: Nerve function can be assessed through various tests, such as:
- Nerve Conduction Studies (NCS): NCS measures the speed and strength of electrical signals along the nerves, helping to determine the extent of nerve damage.
- Electromyography (EMG): EMG assesses the electrical activity of muscles. It can help identify muscle or nerve disorders.
- Sensory and Autonomic Testing: Specialized tests may be conducted to assess sensory and autonomic nerve function, which can help pinpoint the type and extent of neuropathy.
- Cerebrospinal Fluid Analysis: In some cases, a lumbar puncture (spinal tap) may be performed to analyze cerebrospinal fluid for signs of infection or inflammation.
- Nerve Imaging: In some situations, imaging studies like nerve ultrasound or magnetic resonance imaging (MRI) can provide detailed images of nerves and surrounding tissues to help identify structural abnormalities or compression on nerves.
- Nerve Biopsy: In rare cases, a nerve biopsy may be performed, where a small sample of nerve tissue is removed for analysis. This is typically done when other diagnostic methods do not yield a clear diagnosis.
Treatment Options for Neuropathy:

- Medications:
- Pain Relief Medications: Over-the-counter pain relievers (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs) can help manage mild pain.
- Prescription Medications: Doctors may prescribe medications such as gabapentin, pregabalin, or tricyclic antidepressants to alleviate nerve pain.
- Physical Therapy:
- Physical therapists can develop tailored exercise programs to improve muscle strength, balance, and coordination.
- Physical therapy may also include techniques like ultrasound or electrical stimulation for pain relief.
- Lifestyle Changes:
- Blood Sugar Control: For diabetic neuropathy, managing blood sugar levels is crucial.
- Alcohol Reduction: Reducing or eliminating alcohol intake can help with alcoholic neuropathy.
- Foot Care: Regular foot checks and proper footwear are essential for preventing injuries in peripheral neuropathy.
- Complementary Therapies:
- Acupuncture: Some people find relief from neuropathic pain through acupuncture.
- Nutritional Supplements: Supplements like alpha-lipoic acid or B vitamins may help in certain cases.
- Massage Therapy: Massage can improve circulation and provide relief from muscle stiffness.
- Pain Management Techniques:
- Prescription Medications:
- Stronger pain medications like opioids may be considered for severe pain, but their use is closely monitored due to potential side effects and dependency.
- Topical Medications:
- Topical treatments, such as lidocaine patches or capsaicin cream, can be applied directly to the painful area for localized relief.
- Nerve Blocks:
- Nerve block injections can temporarily block pain signals and provide relief, but the effect is often short-term.
- Spinal Cord Stimulation:
- For severe and refractory cases, spinal cord stimulation involves implanting a device that delivers electrical impulses to the spinal cord, interrupting pain signals.
- Transcutaneous Electrical Nerve Stimulation (TENS):
- TENS devices deliver low-level electrical currents to the skin, helping to disrupt pain signals and provide relief.
Living Well with Neuropathy:

- Exercise:
- Engage in regular, low-impact exercises like swimming, walking, or cycling to maintain muscle strength and improve circulation. Consult a physical therapist for a tailored exercise program.
- Nutrition:
- Eat a balanced diet rich in fruits, vegetables, and whole grains. Omega-3 fatty acids found in fish may have anti-inflammatory properties that can benefit neuropathy.
- Pain Journal:
- Keep a pain journal to track your symptoms and identify any patterns or triggers. This can help in managing your condition and discussing your progress with your healthcare provider.
- Support Groups:
- Join a neuropathy support group to connect with others who understand your challenges. Sharing experiences and coping strategies can be incredibly helpful.
- Mind-Body Practices:
- Stress management techniques such as mindfulness meditation and deep breathing can help reduce the perception of pain and improve overall well-being.
If you or a loved one is dealing with neuropathy, remember that early diagnosis and a proactive approach to treatment are essential for living well despite this condition. For personalized guidance and professional medical advice, consult with a healthcare provider who can create a tailored neuropathy management plan. With the right approach, neuropathy doesn’t have to define your life, but rather be a challenge you can successfully navigate.
Disclaimer: This blog post is for informational purposes only and is not a substitute for professional medical advice or treatment. Always consult with a healthcare provider for any health concerns or questions.