How to Maintain Prostate Health: Diet, Exercise, and Lifestyle Tips
Prostate health is a crucial aspect of men’s well-being, and understanding conditions like BPH (Benign Prostatic Hyperplasia) is essential. BPH, a non-cancerous enlargement of the prostate gland, can significantly impact urinary functions as men age.
Benign Prostatic Hyperplasia (BPH) is a common condition that affects a significant number of men as they age. While it is benign, it can lead to uncomfortable symptoms and have a substantial impact on a man’s quality of life. In this post, we will discuss what BPH is, its symptoms, risk factors, diagnosis, and treatment options. Understanding BPH is essential for both men who may be experiencing symptoms and those who want to support their loved ones.
 What is BPH?
What is BPH?
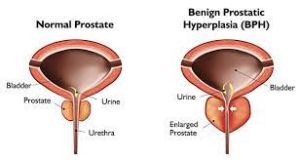
BPH, or Benign Prostatic Hyperplasia, is a non-cancerous enlargement of the prostate gland, which is located just below the bladder. As men age, the prostate gland naturally grows, but in some cases, this enlargement can cause issues.
Common Symptoms of BPH:
Men with BPH may experience a range of urinary symptoms, including:
– Frequent Urination: Needing to urinate more often, especially at night.
– Urgency: A sudden, strong urge to urinate.
– Weak Urine Stream: Difficulty starting urination or a weak urine flow.
– Incomplete Emptying: Feeling like the bladder isn’t fully empty after urination.
– Dribbling: Leaking urine after urination.
Risk Factors for BPH:
Several factors can increase the risk of developing BPH:
– Age: BPH is more common as men get older.
– Family History: If close relatives have had BPH, the risk may be higher.
–Hormonal Changes: Hormones, especially dihydrotestosterone (DHT), play a role in prostate growth.
Diagnosis of BPH:
If you or someone you know is experiencing symptoms, it’s important to consult a healthcare professional. A diagnosis typically involves:
– Medical History: Discussing your symptoms and general health.
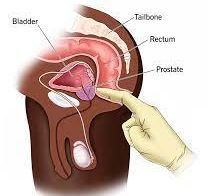
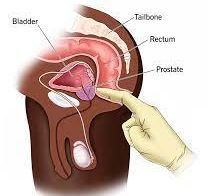
– Physical Examination: The doctor may perform a physical examination, including a digital rectal exam.
– Urine Flow Study: A test to measure the rate of urine flow.
– Prostate-Specific Antigen (PSA) Test: To rule out prostate cancer.
Treatment Options for BPH:
The choice of treatment depends on the severity of symptoms and how much they affect one’s quality of life. Treatment options include:
– Sometimes, mild symptoms may not require immediate treatment, and the condition is monitored over time.
– Prescription drugs can help relax the muscles of the prostate and improve urine flow.
– Minimally Invasive Procedures such as like UroLift and Rezūm, can provide relief with fewer side effects than surgery.
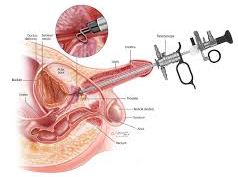
– In severe cases, surgical procedures like TURP (Transurethral Resection of the Prostate) may be recommended.
UroLift

UroLift is a minimally invasive procedure that offers relief from the symptoms of Benign Prostatic Hyperplasia (BPH) without the need for major surgery. Here’s how it works:
During a UroLift procedure, a urologist places small permanent implants into the prostate. These implants are essentially tiny devices that act like “staples” to hold the enlarged prostate tissue away from the urethra, which is the tube through which urine flows.
By holding back the obstructing prostate tissue, UroLift creates an unobstructed channel for urine to pass through. This results in improved urinary flow and reduced BPH-related symptoms, such as frequent urination, urgency, weak urine stream, and incomplete emptying.
A significant advantage of UroLift is its minimal impact on sexual function. Unlike some traditional surgical methods for BPH, UroLift has been associated with a lower risk of sexual side effects. This makes it an attractive option for men who want to maintain their sexual health while addressing BPH.
Recovery after a UroLift procedure is typically quicker and less painful compared to more invasive surgical options. Most men experience relief from BPH symptoms within a few weeks, and they can resume their normal activities sooner.
Rezūm
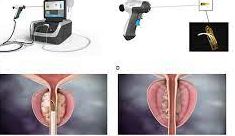
Rezūm is an innovative and minimally invasive BPH treatment that employs the power of steam to reduce the size of the enlarged prostate. Here’s how Rezūm works:
Rezūm uses a small, specialized device that is inserted into the urethra. This device delivers precisely controlled bursts of steam directly into the prostate tissue.
The steam is designed to target and heat the excess prostate tissue, causing cell death and shrinkage. As a result, the prostate begins to decrease in size, relieving the pressure on the urethra.
As the prostate tissue shrinks, urinary symptoms such as frequent urination, urgency, and weak urine flow tend to improve. Many men experience significant relief within a few weeks to a few months after the procedure.
Rezūm is known for its minimal side effects, and it has a low risk of causing sexual dysfunction. It is considered a relatively safe and effective option for BPH treatment.
 Myths and misconceptions surrounding BPH
Myths and misconceptions surrounding BPH
Myth 1: BPH is the same as prostate cancer.
Fact: BPH and prostate cancer are two distinct conditions. BPH is a non-cancerous enlargement of the prostate gland, while prostate cancer is the growth of malignant cells in the prostate. BPH does not increase the risk of developing prostate cancer.
Myth 2: Only older men get BPH.
Fact: While BPH is more common in older men, it can occur in men of all ages, albeit less frequently in younger individuals.
Myth 3: BPH is a sign of poor sexual health.
Fact: BPH is a natural part of the aging process and is not related to sexual activity or sexual health. However, BPH can lead to urinary symptoms that may affect sexual function in some men.
Myth 4: All men with BPH need surgery.
Fact: Surgery is just one of the treatment options for BPH. Many men with mild to moderate symptoms can manage their condition with lifestyle changes, medications, or minimally invasive procedures.
Myth 5: BPH is a life-threatening condition.
Fact: BPH itself is not a life-threatening condition. It may cause bothersome urinary symptoms, but it is not typically life-threatening. However, if left untreated and severe complications develop, it can lead to serious health issues.
Myth 6: There is nothing you can do to prevent BPH.
Fact: While you can’t prevent BPH entirely, certain lifestyle factors like maintaining a healthy diet, staying physically active, and managing other chronic conditions can help reduce the risk of developing BPH or lessen its severity.
Myth 7: BPH always leads to urinary incontinence.
Fact: BPH can cause urinary symptoms, but not all men with BPH experience urinary incontinence. The specific symptoms and their severity can vary from person to person.
Myth 8: Natural remedies are always effective in treating BPH.
Fact: Some natural remedies, such as saw palmetto and beta-sitosterol, have been touted as treatments for BPH. While they may provide relief for some men, their effectiveness varies, and they should be used with caution and under the guidance of a healthcare professional.
Myth 9: BPH Leads to Impotence. Fact: BPH can cause urinary symptoms, but it typically does not lead to impotence or erectile dysfunction. However, some treatments for BPH, like surgery or certain medications, may have side effects that impact sexual function.
Myth 10: Cranberry Juice Can Treat BPH. Fact: Cranberry juice might help prevent urinary tract infections but has not been proven to treat BPH.

Benign Prostatic Hyperplasia is a common condition that can affect the urinary health of older men. Recognizing the symptoms, understanding the risk factors, and seeking timely medical advice can help manage BPH effectively. If you or someone you know is experiencing symptoms, consult a healthcare professional for a proper diagnosis and personalized treatment plan. Remember, BPH is a manageable condition, and with the right care, individuals can lead a full and active life.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.
















