Insulin Functions, Types, and Diabetes Management
Insulin, a vital hormone produced by the pancreas, plays a pivotal role in regulating blood sugar levels and is essential for understanding diabetes management.
Insulin is a vital hormone produced by the pancreas that plays a crucial role in regulating blood sugar levels in the body. In this comprehensive guide, we’ll delve into what you should know about insulin, its functions, types, and how it impacts our health. Additionally, we’ll address the common myths and precautions associated.
 What Is Insulin?
What Is Insulin?
It is a hormone produced by specialized cells in the pancreas called beta cells. Its primary function is to regulate the amount of glucose (sugar) in the bloodstream. When you eat, your blood sugar levels rise as your digestive system breaks down carbohydrates into glucose. It is released into the bloodstream in response to elevated blood sugar levels, allowing glucose to enter cells where it can be used for energy or stored for later use.
Functions
1. It facilitates the uptake of glucose by cells, allowing them to use it for energy.
2. Excess glucose is stored in the liver and muscles as glycogen for future energy needs.
3. It suppresses the liver’s production of glucose, preventing excessive sugar release into the bloodstream.
4. It also promotes the storage of excess glucose as fat in adipose tissue.
There are several types of insulin available, each with unique characteristics:
1. Rapid-Acting: This type begins working within 15 minutes and peaks in about one to two hours. It’s typically taken just before or after meals to manage post-meal blood sugar spikes.
2. Short-Acting: Short-acting insulin starts working within 30 minutes and peaks in two to four hours. It’s usually taken 30 minutes before a meal to help control blood sugar during eating.
3. Intermediate-Acting: This type takes longer to start working (about one to two hours) but has a more extended peak time (four to 12 hours). It’s often used to provide basal insulin coverage between meals and overnight.
4. Long Acting: This type provides a steady release of insulin over an extended period, typically lasting up to 24 hours. It’s used to maintain consistent blood sugar levels throughout the day and night.
Diabetes
In diabetes, the body either doesn’t produce enough insulin (Type 1 diabetes) or can’t use it effectively (Type 2 diabetes). This leads to elevated blood sugar levels, which, if left uncontrolled, can cause various health complications.
– Type 1 Diabetes: Individuals with Type 1 diabetes must take insulin daily through injections or pump since their bodies no longer produce it. Proper insulin management is crucial for survival.
– Type 2 Diabetes: In Type 2 diabetes, the body doesn’t respond well to the insulin it produces. Initially, lifestyle changes and oral medications may be used to manage blood sugar levels, but some individuals may require insulin therapy.
 Delivery Methods
Delivery Methods
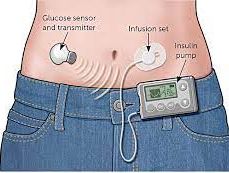
It can be administered through several methods:
- Injections: The most common method involves injecting insulin into the fatty tissue just beneath the skin using a syringe, pen, or pump.
- Pump Therapy: The pumps deliver a continuous supply of insulin throughout the day and can be adjusted as needed.
- Inhalable Insulin: A relatively new option which allows for insulin delivery via inhalation.
 Common Myths
Common Myths
Myth 1: Insulin is only for people with severe diabetes. Fact: It can be used in various types and stages of diabetes management, depending on the individual’s needs.
Myth 2: Insulin causes weight gain. Fact: While it can lead to weight gain in some individuals, proper management and a healthy lifestyle can help minimize this effect.
Myth 3: Insulin cures diabetes. Fact: It is a crucial treatment for diabetes, but it doesn’t cure the condition. It helps manage blood sugar levels effectively.
Myth 4: Insulin Is Only Taken via Injections. Fact: While injections are common, it can also be delivered through pumps or inhalation.
Precautions
- Dosage and Timing: Follow your healthcare provider’s instructions carefully regarding the dosage and timing.
- Blood Sugar Monitoring: Regularly monitor your blood sugar levels to ensure your regimen is effective.
- Hypoglycemia: Be vigilant about low blood sugar (hypoglycemia) symptoms, such as sweating, shakiness, and confusion, especially when using insulin and know how to treat it promptly.
- Injection Site Rotation: If using injections, rotate the injection sites to prevent tissue damage or lipohypertrophy (a buildup of fat under the skin).
- Consult Your Healthcare Provider: Always consult your healthcare provider to determine the most suitable type and regimen for your specific needs, as well as if you have concerns or questions about your insulin therapy.
- Proper Storage: Store the medication as directed; improper storage can affect its effectiveness.
- Dosage Accuracy: Ensure you measure and administer the medication accurately to avoid over- or under-dosage.
Insulin is a critical hormone that regulates blood sugar levels in the body. Understanding its functions, types, and its role in diabetes management is essential for individuals with diabetes and those interested in maintaining overall health. If you have diabetes or suspect you may have a blood sugar-related condition, consult a healthcare provider for personalized guidance and treatment options. Proper insulin management can significantly improve your quality of life and overall well-being while dispelling common myths and following necessary precautions.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.