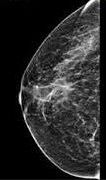
What to Expect During Mammograms: A Step-by-Step Guide
Mammograms are pivotal tools in the realm of breast health. As a cornerstone of breast cancer screening, understanding their significance and debunking associated myths is crucial for every woman’s well-being.

Mammograms are essential tools in the early detection of breast cancer, and yet, many myths and misconceptions surround them. These myths can lead to anxiety and reluctance among women when it comes to scheduling these potentially life-saving screenings. In this blog post, we’ll demystify mammograms by providing you with the facts you should know and debunking some common myths.
 What to Expect Before the Mammogram:
What to Expect Before the Mammogram:
1. Schedule the Appointment: Contact a healthcare facility or mammography center to schedule your mammogram appointment. Make sure to choose a time that works well for you and allows you to relax before and after the procedure.
2. Inform the Technologist: If you are pregnant or suspect you might be pregnant, inform the technologist and the facility before the procedure. Mammograms are generally not recommended during pregnancy due to the use of X-rays.
3. Limit Caffeine: Caffeine can make breasts more sensitive, so it’s a good idea to limit your caffeine intake on the day of the mammogram.
4. Avoid Deodorants and Creams: On the day of the mammogram, it’s best to avoid using deodorants, powders, creams, or perfumes in the underarm or breast area. These substances can interfere with the mammogram images.
The Procedure
Here is a step-by-step overview of how a mammogram is typically performed:
1. Preparation: Before the mammogram, it’s important to inform the technologist if you are pregnant or breastfeeding, as this may affect the procedure. You should also avoid using deodorant, powder, or lotion on your chest or underarms on the day of the exam, as these substances can interfere with the X-ray images.
2. Check-In: When you arrive at the mammography facility, you’ll check in with the receptionist or healthcare staff. You may be asked about your medical history and any breast-related concerns you have.
3. Changing into a Gown: You will be given a gown to wear, usually open at the front. You will need to undress from the waist up, removing clothing and jewelry from the chest area.
4. Positioning: The technologist, who is specially trained in mammography, will guide you to the mammography machine. You will typically stand during the procedure. One breast at a time will be examined, so you’ll need to adjust your position between each image.
5. Compression: Compression is necessary to spread out the breast tissue, allowing for better visualization and reducing X-ray exposure. The technologist will position your breast on the machine’s platform and gently place a clear plastic paddle or compression plate on top of your breast. The pressure applied can be uncomfortable but should not be painful. You’ll be asked to hold your breath briefly while the X-ray is taken.
6. Image Capture: The technologist will step behind a protective barrier and activate the X-ray machine. The X-ray beam will pass through your breast tissue and onto the detector, creating an image of the breast. At least two images are typically taken for each breast, from different angles (usually top-down and side views). Additional images may be taken if the radiologist requires more detail.
7. Repeat for the Other Breast: The same process is repeated for the other breast, with the technologist repositioning you as needed.
8. Review and Completion: Once the images are captured, the technologist will review them to ensure they are of sufficient quality. If additional images are needed, they will be taken at this time. Otherwise, you will be allowed to get dressed.
9. Results:
Your mammogram images will be interpreted by a radiologist, a medical doctor specially trained in reading X-ray images. The results are typically sent to your healthcare provider, who will then discuss the findings with you. You may receive a letter in the mail with your results, or your provider may contact you directly.
The procedure is relatively quick, typically taking around 20 minutes.
What To Expect After the Mammogram:
1. Recovery: After the mammogram, there is typically no downtime, and you can resume your daily activities immediately.
2. Breast Comfort: Some women may experience mild discomfort or tenderness in their breasts following the procedure. This discomfort usually subsides within a few hours to a day. Over-the-counter pain relievers can help if needed.
3. Stay Hydrated: Drink plenty of water to stay hydrated. This can help reduce any potential discomfort or swelling.
4. Avoid Caffeine: Continue to limit caffeine intake for the remainder of the day, as it can contribute to breast tenderness.
5. Follow-Up: You will receive the results of your mammogram within a few weeks. If there are any concerns or additional tests needed, your healthcare provider will discuss them with you. It’s crucial to follow up on any recommendations made by your healthcare team.
6. Regular Screening: Keep track of your mammogram schedule. Many healthcare providers recommend annual mammograms for women aged 40 and older. Staying consistent with your screening appointments is essential for early detection.
7. Breast Self-Exams: Continue to perform regular breast self-exams at home. While mammograms are a crucial part of breast health, self-exams can help you become familiar with your breast tissue and notice any changes between screenings.
8. Talk to Your Healthcare Provider: If you experience any unusual symptoms or changes in your breast health, such as lumps, pain, or nipple discharge, don’t hesitate to contact your healthcare provider for further evaluation.
Some common myths
Myth #1: Mammograms Are Excruciatingly Painful
One of the most prevalent myths about mammograms is that they are incredibly painful. While mammograms may cause some discomfort, they should not be excruciatingly painful. The procedure involves compressing the breast between two plates to get a clear image, which can feel tight or uncomfortable, but it typically lasts only a few seconds per image. Communicate any concerns about discomfort with the technician, as they can often make adjustments to minimize it.
Myth #2: Mammograms Are Not Necessary If You Have No Symptoms
A dangerous myth is that you only need a mammogram if you experience symptoms or have a family history of breast cancer. In reality, breast cancer can develop without any symptoms, and early detection through mammograms can significantly increase the chances of successful treatment. Regular screenings are recommended for women, typically starting at age 40, or earlier if you have a family history or other risk factors.
Myth #3: Mammograms Always Detect Cancer
While mammograms are a valuable screening tool, they are not infallible. They may miss some cancers, particularly in women with dense breast tissue. However, this is why regular screenings are essential. Mammograms can detect many breast cancers at an early, highly treatable stage, which can be a life-saver. False positives, where the test suggests cancer when none is present, can also occur, leading to unnecessary anxiety and follow-up tests. However, the benefits of early detection far outweigh these limitations, as catching cancer in its early stages dramatically improves survival rates.
Myth #4: Mammograms Cause Breast Cancer
Some women worry that the radiation exposure from mammograms can actually cause breast cancer. The amount of radiation used in a mammogram is minimal and considered safe. The risk of developing cancer from the radiation in a mammogram is extremely low and far outweighed by the benefits of early detection.
Myth #5: You Can Skip Mammograms After Menopause
Some women believe that mammograms are no longer necessary after menopause. However, breast cancer risk increases with age, so regular screenings remain important. Discuss with your healthcare provider when and how often you should continue with mammograms based on your individual risk factors.
Myth #6: You Don’t Need Mammograms if You Have Implants
Breast implants do not eliminate the need for mammograms. Special techniques are used to ensure that breast tissue is adequately examined in women with implants. Inform the mammography facility about your implants so they can take appropriate measures.
Myth #7: Mammograms Are Expensive
Mammograms are often covered by health insurance plans, and many countries offer free or subsidized breast cancer screening programs. Cost should not be a barrier to getting this vital test. Check with your healthcare provider and insurance company for coverage details.
Myth #8: Mammograms are Only for Older Women
Another common misconception is that mammograms are only necessary for older women. While breast cancer risk does increase with age, it can affect women of all ages. In fact, some forms of breast cancer can be more aggressive in younger women. It’s important for women to discuss their individual risk factors and screening recommendations with their healthcare provider, but regular mammograms are generally recommended starting at age 40.
Myth #6: Mammograms Are Unnecessary if You Have No Family History of Breast Cancer
While having a family history of breast cancer does increase your risk, the majority of breast cancer cases occur in individuals with no family history. Anyone with breasts is at risk for breast cancer, and regular screening is essential for early detection, regardless of family history.
Mammograms are an invaluable tool in the early detection of breast cancer, and they save countless lives every year. It’s crucial to separate fact from fiction when it comes to mammograms. They are not painful, and they do not cause cancer. Regular screenings, even in the absence of symptoms, can significantly improve the chances of early detection and successful treatment. Don’t let myths and misconceptions prevent you from taking control of your breast health. Regular mammograms are an essential part of breast cancer screening, especially for women over the age of 40 or those with a higher risk of breast cancer. If you have concerns about the procedure or questions about breast cancer screening, it’s a good idea to discuss them with your healthcare provider. It’s essential to follow your healthcare provider’s recommendations for screening and to discuss any concerns or questions you have about the procedure with your healthcare team. Talk to your healthcare provider about when you should start mammograms and how often you should have them based on your individual risk factors. Remember, early detection is key to improving breast cancer outcomes. Your health and peace of mind are worth it.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.