
Pressure Ulcer Prevention: The Importance of Regular Movement and Repositioning
Pressure ulcers, commonly known as bedsores, pose significant risks, especially for individuals with limited mobility. Understanding the importance of prevention and recognizing early signs can make a profound difference in one’s quality of life.

Pressure ulcers, also known as bedsores or pressure sores, are wounds that typically form on bony areas of the body, such as the heels, elbows, hips, and tailbone. They are painful and often preventable skin injuries that can affect individuals of all ages, especially those with limited mobility. These sores develop when pressure is consistently applied to a specific area of the body, reducing blood flow and causing the skin and underlying tissues to break down.
Causes Of Pressure Ulcers
Pressure ulcers develop due to sustained pressure on the skin and underlying tissues. When this pressure exceeds the blood flow to a particular area of the body, it can result in tissue damage and the formation of an ulcer. Common causes include:
1. Immobility: Individuals who are bedridden or have limited mobility are at a higher risk because they frequently remain in one position for extended periods.
2. Friction and Shear: Rubbing or sliding of the skin against a surface (friction) and the separation of tissue layers as they slide in opposite directions (shear) can damage the skin’s integrity, making it more susceptible to pressure ulcer development.
3. Poor Nutrition: Malnutrition or dehydration can weaken the skin and reduce its ability to heal, increasing the risk of ulcers.
4. Medical Conditions: Conditions like diabetes, vascular disease, or neurological disorders can impair blood flow and sensation, making skin more vulnerable to injury.
5. Age: Older adults are more prone to ulcers due to changes in skin elasticity and decreased mobility.
Risk Factors for Pressure Ulcers
Several risk factors increase the likelihood of developing ulcers. Understanding these risk factors is essential for prevention:
- Limited Mobility: Individuals who are bedridden, use wheelchairs, or have difficulty changing positions are more susceptible to ulcers.
- Reduced Sensation: People with impaired sensation due to conditions like diabetes or spinal cord injuries may not feel the discomfort or pain caused by pressure, making them less likely to shift positions to relieve it.
- Inadequate Nutrition: Poor nutrition can weaken the skin and reduce its ability to withstand pressure and heal wounds.
- Advanced Age: Older adults may have thinner skin, reduced tissue elasticity, and more fragile blood vessels, making them more prone to pressure ulcers.
- Incontinence: Moisture from urine or feces can weaken the skin and make it more susceptible to damage.
The Stages of Pressure Ulcers:
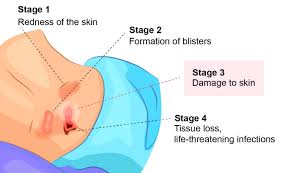
Pressure ulcers progress through several stages, from mild redness and skin damage to open sores that can extend deep into the tissue. The severity of an ulcer depends on various factors, including the individual’s overall health and the quality of care received.
- Stage I: At this stage, the skin may appear red or discolored, but it’s not broken. It’s usually warm to the touch and may be painful.
- Stage 2: In this stage, the outer layer of skin (epidermis) and the underlying layer (dermis) are damaged or lost. The sore may look like an open blister or a shallow, reddish-pink crater.
- Stage 3: Here, the damage extends through the dermis and into the subcutaneous (fatty) tissue. The wound may appear as a deep crater with a yellowish dead tissue at the base.
- Stage 4: This is the most severe stage, involving extensive damage through all skin layers, potentially affecting muscle and even bone. The wound is deep, extending to muscle, bone, or other underlying structures and there’s often blackened, dead tissue. Infections and complications are more likely in this stage.
Prevention Strategies
Preventing pressure ulcers involves a combination of strategies to reduce pressure, maintain skin health, and address risk factors. Here are some key prevention strategies:
- Frequent Repositioning: If you or someone you care for has limited mobility, bedridden or use a wheelchair; change positions regularly at least every two hours, if possible, to relieve pressure on vulnerable areas. Use cushions or pillows to reduce pressure on bony areas and to help distribute pressure evenly. Change positions frequently. Use cushions or padding.
- Skin Care: Keep the skin clean and well-moisturized. Moisturize to prevent skin dryness and maintain cleanliness to reduce the risk of infection. Use mild soaps and avoid harsh scrubbing. Check the skin regularly for signs of redness or damage.
- Proper Nutrition: Maintain a balanced diet rich in protein, vitamins and minerals to support skin health, tissue repair and overall well-being. Consult a healthcare professional for dietary advice.
- Manage Moisture: If incontinence is a concern, use absorbent products and change them promptly. Keep the skin dry and use protective creams or ointments if necessary.
- Pressure-Relieving Devices: Consider using specialized cushions, mattresses, or support surfaces designed to reduce pressure on vulnerable areas.
- Education: Educate yourself and caregivers about pressure ulcer prevention, including the importance of early detection and appropriate interventions.
- Regular Checkups: If you are at risk for pressure ulcers, consult with a healthcare professional for regular skin assessments and guidance on prevention.
- Manage Incontinence: If applicable, manage incontinence promptly to prevent moisture-related skin issues.
- Regular Skin Inspections: Check your skin daily for any signs of redness, irritation, discoloration, or damage, and seek medical attention at the first sign of trouble.
- Mobility: Encourage regular movement and exercise, even if limited, to improve circulation and muscle tone.

Management and Treatment
If you or a loved one develop a pressure ulcer, it’s crucial to seek medical attention promptly. Treatment will vary depending on the stage and severity of the ulcer but may include:
- Wound Cleaning: The wound should be cleaned to remove dead tissue, bacteria, and debris.
- Dressing Changes: Dressings may be applied to keep the wound clean and promote healing.
- Pressure Relief: Continue to relieve pressure on the affected area through repositioning and the use of specialized support surfaces.
- Nutritional Support: Adequate nutrition is crucial for healing. Dietary changes or supplements may be recommended.
- Infection Control: Antibiotics may be necessary if an infection develops.
- Surgery: In severe cases, surgical intervention may be required to remove dead tissue or repair damaged areas.
Myths and Misconceptions about Pressure Ulcers
1. They Only Affect the Elderly: While pressure ulcers are more common among older adults, they can affect people of all ages, especially those with limited mobility due to injury, illness, or disability.
2. They Always Develop Quickly: Pressure ulcers can develop gradually over time, especially in individuals with chronic health conditions. Regular skin checks are essential to catch them early.
3. They Are Always Painful: While pressure ulcers can be painful, especially in later stages, some individuals with reduced sensation may not feel pain. Lack of pain does not mean there is no risk.
4. They Always Heal on Their Own: Pressure ulcers may require specialized medical care, including wound debridement, dressings, and sometimes surgery, to heal properly.
5. They Are Contagious: Pressure ulcers are not contagious; they result from a combination of factors, including pressure, friction, and moisture, and cannot be transmitted from one person to another.
6. Once Healed, They Won’t Recur: Individuals who have had pressure ulcers are at a higher risk of developing them again, especially if preventive measures are not continued.
Pressure ulcers can be painful, debilitating, and costly to treat. However, with proper awareness, education, and preventive measures, they can often be avoided. By understanding the causes, recognizing the stages, and implementing effective prevention strategies, we can work together to protect the skin and overall well-being of those at risk for pressure ulcers.
Disclaimer: The information provided in this content is for general informational purposes only. It is not intended as medical or healthcare advice, diagnosis, or treatment. Always seek the advice of a qualified healthcare professional with any questions you may have regarding a medical condition or healthcare decisions.
















